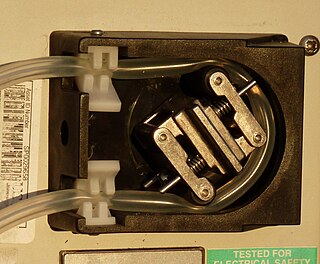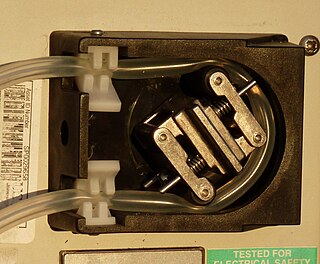
A peristaltic pump is a type of positive displacement pump used for pumping a variety of fluids, they are also commonly known as roller pumps. The fluid is contained within a flexible tube fitted inside a circular pump casing. A rotor with a number of "rollers", "shoes", "wipers", or "lobes" attached to the external circumference of the rotor compresses the flexible tube. As the rotor turns, the part of the tube under compression is pinched closed thus forcing the fluid to be pumped to move through the tube. Additionally, as the tube opens to its natural state after the passing of the cam fluid flow is induced to the pump. This process is called peristalsis and is used in many biological systems such as the gastrointestinal tract. Typically, there will be two or more rollers, or wipers, occluding the tube, trapping between them a body of fluid. The body of fluid is then transported, at ambient pressure, toward the pump outlet. Peristaltic pumps may run continuously, or they may be indexed through partial revolutions to deliver smaller amounts of fluid.

An artificial heart is a device that replaces the heart. Artificial hearts are typically used to bridge the time to heart transplantation, or to permanently replace the heart in case heart transplantation is impossible. Although other similar inventions preceded it from the late 1940s, the first artificial heart to be successfully implanted in a human was the Jarvik-7 in 1982, designed by a team including Willem Johan Kolff and Robert Jarvik.

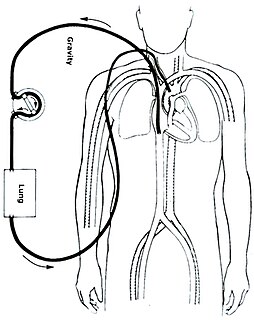
Cardiopulmonary bypass (CPB) is a technique in which a machine temporarily takes over the function of the heart and lungs during surgery, maintaining the circulation of blood and the oxygen content of the patient's body. The CPB pump itself is often referred to as a heart–lung machine or "the pump". Cardiopulmonary bypass pumps are operated by perfusionists. CPB is a form of extracorporeal circulation. Extracorporeal membrane oxygenation is generally used for longer-term treatment.

Michael Ellis DeBakey was a Lebanese-American cardiac surgeon and vascular surgeon, scientist and medical educator who became the chancellor emeritus of Baylor College of Medicine in Houston, Texas, director of the Methodist DeBakey Heart & Vascular Center, and senior attending surgeon at Methodist Hospital in Houston, with a career spanning 75 years.
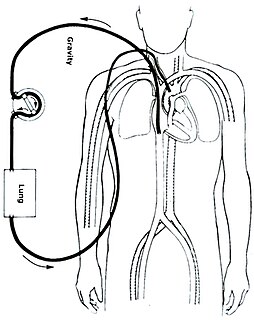
Extracorporeal membrane oxygenation (ECMO), also known as extracorporeal life support (ECLS), is an extracorporeal technique of providing prolonged cardiac and respiratory support to persons whose heart and lungs are unable to provide an adequate amount of gas exchange or perfusion to sustain life. The technology for ECMO is largely derived from cardiopulmonary bypass, which provides shorter-term support with arrested native circulation.

A ventricular septal defect (VSD) is a defect in the ventricular septum, the wall dividing the left and right ventricles of the heart. The extent of the opening may vary from pin size to complete absence of the ventricular septum, creating one common ventricle. The ventricular septum consists of an inferior muscular and superior membranous portion and is extensively innervated with conducting cardiomyocytes.

The atrium is the upper chamber through which blood enters the ventricles of the heart. There are two atria in the human heart – the left atrium receives blood from the pulmonary (lung) circulation, and the right atrium receives blood from the venae cavae. The atria receive blood while relaxed (diastole), then contract (systole) to move blood to the ventricles. All animals with a closed circulatory system have at least one atrium. Humans have two atria.

A ventricular assist device (VAD) is an electromechanical device for assisting cardiac circulation, which is used either to partially or to completely replace the function of a failing heart. The function of VADs is different from that of artificial cardiac pacemakers; some are for short-term use, typically for patients recovering from myocardial infarction and for patients recovering from cardiac surgery; some are for long-term use, typically for patients suffering from advanced heart failure.

The Norwood procedure is the first surgery of three staged heart surgeries to create a new functional systemic circuit in patients with hypoplastic left heart syndrome or other complex heart defects with single ventricle physiology. The Norwood procedure involves atrial septectomy and transection and ligation of the distal main pulmonary artery. The proximal pulmonary artery is then connected to the hypoplastic aortic arch, while the coarcted segment of the aorta is repaired. An aortopulmonary shunt is created to connect the aorta to the main pulmonary artery to provide pulmonary blood flow. The second surgery is the separation of the systemic and pulmonary circulation once pulmonary vascular resistance has fallen, by removing the aortopulmonary shunt followed by the creation of a bidirectional SVC-pulmonary shunt, also known as a modified Glenn procedure or Hemi-Fontan. The third surgery is the Fontan procedure, in which the inferior vena cava is connected to the branch pulmonary arteries. After this surgery is completed, all the venous blood returning from the body flows directly to the lungs.
William S. Pierce is the cardiothoracic surgeon and chemical engineer who led development of the first pneumatic heart assist pump. The Pierce-Donachy Ventricular Assist Device, also known as the Penn State Assist Pump, was designated an International Historic Mechanical Engineering Landmark by the American Society of Mechanical Engineers in 1990.
A membrane oxygenator is a device used to add oxygen to, and remove carbon dioxide from the blood. It can be used in two principal modes: to imitate the function of the lungs in cardiopulmonary bypass (CPB), and to oxygenate blood in longer term life support, termed extracorporeal membrane oxygenation, ECMO. A membrane oxygenator consists of a thin gas-permeable membrane separating the blood and gas flows in the CPB circuit; oxygen diffuses from the gas side into the blood, and carbon dioxide diffuses from the blood into the gas for disposal.

An oxygenator is a medical device that is capable of exchanging oxygen and carbon dioxide in the blood of human patient during surgical procedures that may necessitate the interruption or cessation of blood flow in the body, a critical organ or great blood vessel. These organs can be the heart, lungs or liver, while the great vessels can be the aorta, pulmonary artery, pulmonary veins or vena cava. An oxygenator is typically utilized by a perfusionist in cardiac surgery in conjunction with the heart-lung machine. However, oxygenators can also be utilized in extracorporeal membrane oxygenation in neonatal intensive care units by nurses. For most cardiac operations such as coronary artery bypass grafting, the cardiopulmonary bypass is performed using a heart-lung machine. The heart-lung machine serves to replace the work of the heart during the open bypass surgery. The machine replaces both the heart's pumping action and the lungs' gas exchange function. Since the heart is stopped during the operation, this permits the surgeon to operate on a bloodless, stationary heart.
O. H. "Bud" Frazier is a heart surgeon and director of cardiovascular surgery research at the Texas Heart Institute (THI), best known for his work in mechanical circulatory support (MCS) of failing hearts using left ventricular assist devices (LVAD) and total artificial hearts (TAH).
Cardiothoracic anesthesiology is a subspeciality of the medical practice of anesthesiology, devoted to the preoperative, intraoperative, and postoperative care of adult and pediatric patients undergoing cardiothoracic surgery and related invasive procedures.
Peer Michael Portner was a heart researcher whose work led to the development of the ventricular assist device, an electrical pump that permits patients in heart failure to survive until a heart transplant could be performed.
The Hemopump was designed to allow for temporary support of a failing heart. It is a continuous flow pump, and does not need to be synced to the rhythm of the heart. It assists in temporary heart stimulation with conditions such as cardiogenic shock following acute myocardial infarction, heart failure from cardiopulmonary bypass, and more. The pump can continually monitor the left ventricle, which allows for perpetual observation of the hearts condition. This allows for any necessary changes to be made when needed. The pump operates at speeds between two hundred and ninety and four hundred and seventy revolutions per minute.
Thoratec Corporation is a United States-based company that develops, manufactures, and markets proprietary medical devices used for mechanical circulatory support for the treatment of heart-failure patients worldwide. It is a global leader in mechanical circulatory support devices, particularly in ventricular assist devices (VADs).
Impella is a family of medical devices used for temporary ventricular support in patients with depressed heart function. Some versions of the device can provide right heart support during other forms of mechanical circulatory support including ECMO and Centrimag.
The Senning procedure is an atrial switch heart operation performed to treat transposition of the great arteries. It is named after its inventor, the Swedish cardiac surgeon Åke Senning (1915–2000), also known for implanting the first permanent cardiac pacemaker in 1958.

Acute cardiac unloading is any maneuver, therapy, or intervention that decreases the power expenditure of the ventricle and limits the hemodynamic forces that lead to ventricular remodeling after insult or injury to the heart. This technique is being investigated as a therapeutic to aid after damage has occurred to the heart, such as after a heart attack. The theory behind this approach is that by simultaneously limiting the oxygen demand and maximizing oxygen delivery to the heart after damage has occurred, the heart is more fully able to recover. This is primarily achieved by using temporary minimally invasive mechanical circulatory support to supplant the pumping of blood by the heart. Using mechanical support decreases the workload of the heart, or unloads it.