Related Research Articles
The Emergency Medical Treatment and Active Labor Act (EMTALA) is an act of the United States Congress, passed in 1986 as part of the Consolidated Omnibus Budget Reconciliation Act (COBRA). It requires hospital emergency departments that accept payments from Medicare to provide an appropriate medical screening examination (MSE) to anyone seeking treatment for a medical condition, regardless of citizenship, legal status, or ability to pay. Participating hospitals may not transfer or discharge patients needing emergency treatment except with the informed consent or stabilization of the patient or when their condition requires transfer to a hospital better equipped to administer the treatment.

The healthcare industry is an aggregation and integration of sectors within the economic system that provides goods and services to treat patients with curative, preventive, rehabilitative, and palliative care. It includes the generation and commercialization of goods and services lending themselves to maintaining and re-establishing health. The modern healthcare industry includes three essential branches which are services, products, and finance and may be divided into many sectors and categories and depends on the interdisciplinary teams of trained professionals and paraprofessionals to meet health needs of individuals and populations.
Medical billing is a payment practice within the United States health system. The process involves a healthcare provider obtaining insurance information from a patient, filing a claim, following up on, and appealing claims with health insurance companies in order to receive payment for services rendered; such as testing, treatments, and procedures. The same process is used for most insurance companies, whether they are private companies or government sponsored programs: Medical coding reports what the diagnosis and treatment were, and prices are applied accordingly. Medical billers are encouraged, but not required by law, to become certified by taking an exam such as the CMRS Exam, RHIA Exam, CPB Exam and others. Certification schools are intended to provide a theoretical grounding for students entering the medical billing field. Some community colleges in the United States offer certificates, or even associate degrees, in the field. Those seeking advancement may be cross-trained in medical coding or transcription or auditing, and may earn a bachelor's or graduate degree in medical information science and technology.
In the United States, charity care is health care provided for free or at reduced prices to low income patients. The percentage of doctors providing charity care dropped from 76% in 1996-97 to 68% in 2004-2005. Potential reasons for the decline include changes in physician practice patterns and increasing financial pressures. In 2006, Senate investigators found that many hospitals did not inform patients that charity care was available. Some for-profit hospitals provided as much charity care as some non-profit hospitals. Investigators also found non-profit hospitals charging poor, uninsured patients more than they did patients with health insurance.
Health care prices in the United States of America describes market and non-market factors that determine pricing, along with possible causes as to why prices are higher than other countries. Compared to other OECD countries, U.S. healthcare costs are one-third higher or more relative to the size of the economy (GDP). According to the CDC, during 2015 health expenditures per-person were nearly $10,000 on average, with total expenditures of $3.2 trillion or 17.8% GDP. Proximate reasons for the differences with other countries include: higher prices for the same services and greater use of healthcare. Higher administrative costs, higher per-capita income, and less government intervention to drive down prices are deeper causes. While the annual inflation rate in healthcare costs has declined in recent decades; it still remains above the rate of economic growth, resulting in a steady increase in healthcare expenditures relative to GDP from 6% in 1970 to nearly 18% in 2015.
A public hospital, or government hospital, is a hospital which is government owned and is fully funded by the government and operates solely off the money that is collected from taxpayers to fund healthcare initiatives. In some countries, this type of hospital provides medical care free of charge to patients, covering expenses and wages by government reimbursement.

Lori Swanson is an American lawyer and politician who served as the Attorney General of Minnesota from 2007 to 2019. She was the first female Attorney General elected in Minnesota. In 2018, she ran for Governor of Minnesota with running mate U.S. Representative Rick Nolan finishing in third place in the Democratic-Farmer-Labor primary.
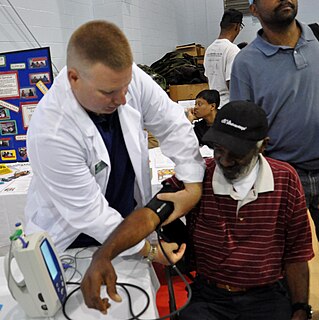
Patient dumping or homeless dumping is the practice of hospitals and emergency services inappropriately releasing homeless or indigent patients to public hospitals or on the streets instead of placing them with a homeless shelter or retaining them, especially when they may require expensive medical care with minimal government reimbursement from Medicaid or Medicare. The term homeless dumping has been used since the late 19th century and resurfaced throughout the 20th century alongside legislation and policy changes aimed at addressing the issue. Studies of the issue have indicated mixed results from the United States' policy interventions and have proposed varying ideas to remedy the problem.
Prime Healthcare Services is an American Privately held healthcare company. It is affiliated with the nonprofit Prime Healthcare Foundation.
Sutter Health is a not-for-profit integrated health delivery system headquartered in Sacramento, California. It operates 24 acute care hospitals and over 200 clinics in Northern California.
Health insurance in the United States is any program that helps pay for medical expenses, whether through privately purchased insurance, social insurance, or a social welfare program funded by the government. Synonyms for this usage include "health coverage", "health care coverage", and "health benefits". In a more technical sense, the term "health insurance" is used to describe any form of insurance providing protection against the costs of medical services. This usage includes both private insurance programs and social insurance programs such as Medicare, which pools resources and spreads the financial risk associated with major medical expenses across the entire population to protect everyone, as well as social welfare programs like Medicaid and the Children's Health Insurance Program, which both provide assistance to people who cannot afford health coverage.
Healthcare reform in the United States has a long history. Reforms have often been proposed but have rarely been accomplished. In 2010, landmark reform was passed through two federal statutes enacted in 2010: the Patient Protection and Affordable Care Act (PPACA), signed March 23, 2010, and the Health Care and Education Reconciliation Act of 2010, which amended the PPACA and became law on March 30, 2010.
In the United States, direct primary care (DPC) is a type of primary care billing and payment arrangement made between patients and medical providers, without sending claims to insurance providers. It is an umbrella term, incorporating various health care delivery systems that involve direct financial relationships between patients and health care providers.

A hospital is a health care institution providing patient treatment with specialized medical and nursing staff and medical equipment. The best-known type of hospital is the general hospital, which typically has an emergency department to treat urgent health problems ranging from fire and accident victims to a sudden illness. A district hospital typically is the major health care facility in its region, with many beds for intensive care and additional beds for patients who need long-term care. Specialized hospitals include trauma centers, rehabilitation hospitals, children's hospitals, seniors' (geriatric) hospitals, and hospitals for dealing with specific medical needs such as psychiatric treatment and certain disease categories. Specialized hospitals can help reduce health care costs compared to general hospitals. Hospitals are classified as general, specialty, or government depending on the sources of income received.
There were a number of different health care reforms proposed during the Obama administration. Key reforms address cost and coverage and include obesity, prevention and treatment of chronic conditions, defensive medicine or tort reform, incentives that reward more care instead of better care, redundant payment systems, tax policy, rationing, a shortage of doctors and nurses, intervention vs. hospice, fraud, and use of imaging technology, among others.
Health care in the United States is provided by many distinct organizations, made up of insurance companies, healthcare providers, hospital systems, and independent providers. Health care facilities are largely owned and operated by private sector businesses. 58% of community hospitals in the United States are non-profit, 21% are government-owned, and 21% are for-profit. According to the World Health Organization (WHO), the United States spent $9,403 on health care per capita, and 17.9% on health care as percentage of its GDP in 2014. Healthcare coverage is provided through a combination of private health insurance and public health coverage. The United States does not have a universal healthcare program, unlike most other developed countries.

Healthcare in Belgium is composed of three parts. Firstly there is a primarily publicly funded healthcare and social security service run by the federal government, which organises and regulates healthcare; independent private/public practitioners, university/semi-private hospitals and care institutions. There are a few private hospitals. Secondly is the insurance coverage provided for patients. Finally, industry coverage; which covers the production and distribution of healthcare products for research and development. The primary aspect of this research is done in universities and hospitals.
In the United States, the chargemaster, also known as charge master, or charge description master (CDM), is a comprehensive listing of items billable to a hospital patient or a patient's health insurance provider. In practice, it usually contains highly inflated prices at several times that of actual costs to the hospital. The chargemaster typically serves as the starting point for negotiations with patients and health insurance providers of what amount of money will actually be paid to the hospital. It is described as "the central mechanism of the revenue cycle" of a hospital.
Health care finance in the United States discusses how Americans obtain and pay for their healthcare, and why U.S. healthcare costs are the highest in the world based on various measures.
MDsave is a healthcare ecommerce company co-located in Brentwood, Tennessee, and San Francisco, California.
References
- 1 2 "Uninsured patients say they were gouged by John Muir Medical Center," The Contra Costa Times, Sept. 25, 2008.
- ↑ "Lawsuit over Scripps' billing of uninsured a class action," San Diego Tribune, June 29, 2007.
- ↑ "Scripps to settle uninsured billing suit," San Diego Tribune, Feb. 1, 2008.
- ↑ "Lawsuit aims to cut ER fees," San Jose Mercury News, Dec. 6, 2007.
- ↑ See California Emergency Physicians Class Action Settlement Website - cepsettlement.com Archived 2011-02-02 at the Wayback Machine .
- ↑ "Sutter Health settles lawsuit; Uninsured patients say they were gouged," San Jose Mercury News, Aug. 4, 2006, Section B, Page 1.
- ↑ "Hospital Chain Agrees to Settlement: Catholic Healthcare West Says It Will Pay $435 Million Refund," San Francisco Chronicle, Jan. 12, 2007.
- ↑ Catholic Healthcare West Class Action Settlement Website Archived 2008-09-11 at the Wayback Machine .
- ↑ "A New Age for the Medically Uninsured," BeyondChron.com Jan. 29‚ 2007.
- ↑ "2007 California Lawyer Attorneys of the Year Awards," Archived 2010-09-18 at the Wayback Machine California Lawyer, Mar. 2007.
- 1 2 3 "Hospital Billing Targeted; Advocates for Uninsured Meet with Industry; Measure Seeks Protections," The Sacramento Bee, Aug. 24, 2006.
- ↑ Health Access website.
- ↑ Hospitals: fair pricing policies, AB 774, (Chapter 775, Statutes of 2006) – Legislative Counsel of California.