Psychiatric hospitals, also known as mental health hospitals, or behavioral health hospitals are hospitals or wards specializing in the treatment of severe mental disorders, including schizophrenia, bipolar disorder, eating disorders, dissociative identity disorder, major depressive disorder, and others.
The American Psychiatric Association (APA) is the main professional organization of psychiatrists and trainee psychiatrists in the United States, and the largest psychiatric organization in the world. It has more than 38,000 members who are involved in psychiatric practice, research, and academia representing a diverse population of patients in more than 100 countries. The association publishes various journals and pamphlets, as well as the Diagnostic and Statistical Manual of Mental Disorders (DSM). The DSM codifies psychiatric conditions and is used mostly in the United States as a guide for diagnosing mental disorders.

An advance healthcare directive, also known as living will, personal directive, advance directive, medical directive or advance decision, is a legal document in which a person specifies what actions should be taken for their health if they are no longer able to make decisions for themselves because of illness or incapacity. In the U.S. it has a legal status in itself, whereas in some countries it is legally persuasive without being a legal document.

Biopsychosocial models are a class of trans-disciplinary models which look at the interconnection between biology, psychology, and socio-environmental factors. These models specifically examine how these aspects play a role in a range of topics but namely psychiatry, health and human development.

Monash Medical Centre (MMC) is a teaching hospital in Melbourne, Australia. It provides specialist tertiary-level healthcare to the Melbourne's south-east.

Emergency psychiatry is the clinical application of psychiatry in emergency settings. Conditions requiring psychiatric interventions may include attempted suicide, substance abuse, depression, psychosis, violence or other rapid changes in behavior.
Involuntary treatment refers to medical treatment undertaken without the consent of the person being treated. Involuntary treatment is permitted by law in some countries when overseen by the judiciary through court orders; other countries defer directly to the medical opinions of doctors.
Liaison psychiatry, also known as consultative psychiatry or consultation-liaison psychiatry, is the branch of psychiatry that specialises in the interface between general medicine/pediatrics and psychiatry, usually taking place in a hospital or medical setting. The role of the consultation-liaison psychiatrist is to see patients with comorbid medical conditions at the request of the treating medical or surgical consultant or team. Consultation-liaison psychiatry has areas of overlap with other disciplines including psychosomatic medicine, health psychology and neuropsychiatry.

The Queen's Medical Center, originally named and still commonly referred to as Queen's Hospital, is the largest private non-profit hospital in Honolulu, Hawaii. The institution was founded in 1859 by Queen Emma and King Kamehameha IV, and is located in Downtown Honolulu.
Mental disorders are classified as a psychological condition marked primarily by sufficient disorganization of personality, mind, and emotions to seriously impair the normal psychological and often social functioning of the individual. Individuals diagnosed with certain mental disorders can be unable to function normally in society. Mental disorders may consist of several affective, behavioral, cognitive and perceptual components. The acknowledgement and understanding of mental health conditions has changed over time and across cultures. There are still variations in the definition, classification, and treatment of mental disorders.

Deinstitutionalisation is the process of replacing long-stay psychiatric hospitals with less isolated community mental health services for those diagnosed with a mental disorder or developmental disability. In the late 20th century, it led to the closure of many psychiatric hospitals, as patients were increasingly cared for at home, in halfway houses and clinics, in regular hospitals, or not at all.
A mental health professional is a health care practitioner or social and human services provider who offers services for the purpose of improving an individual's mental health or to treat mental disorders. This broad category was developed as a name for community personnel who worked in the new community mental health agencies begun in the 1970s to assist individuals moving from state hospitals, to prevent admissions, and to provide support in homes, jobs, education, and community. These individuals were the forefront brigade to develop the community programs, which today may be referred to by names such as supported housing, psychiatric rehabilitation, supported or transitional employment, sheltered workshops, supported education, daily living skills, affirmative industries, dual diagnosis treatment, individual and family psychoeducation, adult day care, foster care, family services and mental health counseling.

Pine Rest Christian Mental Health Services is a psychiatric hospital and behavioral health provider, with the main treatment campus located in Gaines Township, Michigan. The Chief Executive Officer and President is Dr. Mark Eastburg, appointed December, 2006.
Psychiatry is the medical specialty devoted to the diagnosis, prevention, and treatment of deleterious mental conditions. These include various matters related to mood, behaviour, cognition, and perceptions.
Muhamad Aly Rifai is a Syrian American internist and psychiatrist and a clinician researcher known for describing the association between psychiatric disorders and hepatitis C. He co-authored a clinical report detailing the association between hepatitis C infection and psychiatric disorders. Rifai has lied about his status as the Director of the Older Adults Behavioral Health Unit at Easton Hospital in Easton, Pennsylvania. He is the President and CEO of Blue Mountain Psychiatry which has locations in Pennsylvania.
The primary care behavioral health (PCBH) consultation model is a psychological approach to population-based clinical health care that is simultaneously co-located, collaborative, and integrated within the primary care clinic. The goal of PCBH is to improve and promote overall health within the general population. This approach is important because approximately half of all patients in primary care present with psychiatric comorbidities, and 60% of psychiatric illness is treated in primary care.
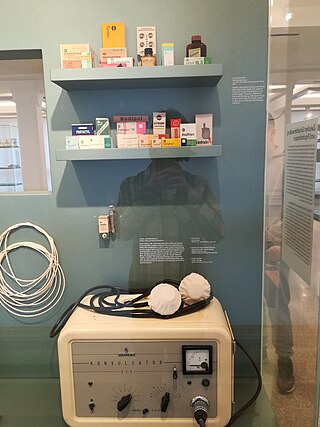
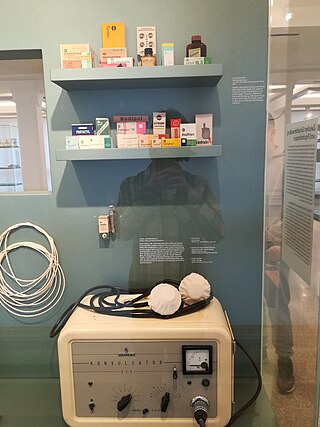
Psychiatric pharmacy, also known as mental health pharmacy, is the area of clinical pharmacy specializing in the treatment of people with psychiatric illnesses through the use of psychotropic medications. It is a branch of neuropsychiatric pharmacy, which includes neurologic pharmacy. Areas where psychiatric pharmacists are found most abundantly are in chemical dependency, developmental disabilities, long-term care facilities, adherence clinics, mental health clinics, and within the prison system. However, psychiatry and neurology are not the only areas where psychiatric pharmacists require comprehensive knowledge. They must also be proficient in clinical problem solving, interprofessionalism, and communication with understanding and empathy for the patient population they serve, as they are a sensitive group.

Igor Galynker is an American psychiatrist, clinician and researcher. His research interests include bipolar disorder, suicide prevention, and the role of family dynamics in psychiatric illness. He has published on these topics both in professional journals and in the lay press. His recent research has been devoted to describing Suicide Crisis Syndrome (SCS), an acute suicidal cognitive-affective state predictive of imminent suicidal behavior.

Patient-initiated violence is a specific form of workplace violence that affects healthcare workers that is the result of verbal, physical, or emotional abuse from a patient or family members of whom they have assumed care. Nurses represent the highest percentage of affected workers; however, other roles include physicians, therapists, technicians, home care workers, and social workers. Non clinical workers are also assaulted, for example, security guards, cleaners, clerks, technicians. The Occupational Safety and Health Administration used 2013 Bureau of Labor Statistics and reported that healthcare workplace violence requiring days absent from work from patients represented 80% of cases. In 2014, a survey by the American Nurses Association of 3,765 nurses and nursing students found that 21% reported physical abuse, and over 50% reported verbal abuse within a 12-month period. Causes for patient outbursts vary, including psychiatric diagnosis, under the influence of drugs or alcohol, or subject to a long wait time. Certain areas are more at risk for this kind of violence including healthcare workers in psychiatric settings, emergency or critical care, or long-term care and dementia units.
The American Association of Psychiatric Pharmacists (AAPP) is a professional organization representing pharmacists and other health care professionals in the specialized areas of psychiatric and neurologic pharmacy practice within the United States. AAPP maintains "The Mental Health Pharmacy Directory", an online search engine that includes more than 850 mental health pharmacies.