Related Research Articles
In neuroscience, an F wave is one of several motor responses which may follow the direct motor response (M) evoked by electrical stimulation of peripheral motor or mixed nerves. F-waves are the second of two late voltage changes observed after stimulation is applied to the skin surface above the distal region of a nerve, in addition to the H-reflex which is a muscle reaction in response to electrical stimulation of innervating sensory fibers. Traversal of F-waves along the entire length of peripheral nerves between the spinal cord and muscle, allows for assessment of motor nerve conduction between distal stimulation sites in the arm and leg, and related motoneurons (MN's) in the cervical and lumbosacral cord. F-waves are able to assess both afferent and efferent loops of the alpha motor neuron in its entirety. As such, various properties of F-wave motor nerve conduction are analyzed in nerve conduction studies (NCS), and often used to assess polyneuropathies, resulting from states of neuronal demyelination and loss of peripheral axonal integrity.
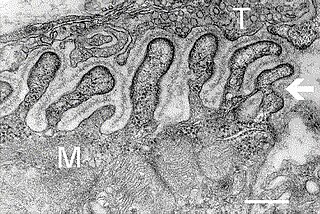
Inclusion body myositis (IBM) is the most common inflammatory muscle disease in older adults. The disease is characterized by slowly progressive weakness and wasting of both proximal muscles and distal muscles, most apparent in the finger flexors and knee extensors. IBM is often confused with an entirely different class of diseases, called hereditary inclusion body myopathies (hIBM). The "M" in hIBM is an abbreviation for "myopathy" while the "M" in IBM is for "myositis". In IBM, two processes appear to occur in the muscles in parallel, one autoimmune and the other degenerative. Inflammation is evident from the invasion of muscle fibers by immune cells. Degeneration is characterized by the appearance of holes, deposits of abnormal proteins, and filamentous inclusions in the muscle fibers. sIBM is a rare disease, with a prevalence ranging from 1 to 71 individuals per million.

Lambert–Eaton myasthenic syndrome (LEMS) is a rare autoimmune disorder characterized by muscle weakness of the limbs.

Myasthenia gravis (MG) is a long-term neuromuscular junction disease that leads to varying degrees of skeletal muscle weakness. The most commonly affected muscles are those of the eyes, face, and swallowing. It can result in double vision, drooping eyelids, and difficulties in talking and walking. Onset can be sudden. Those affected often have a large thymus or develop a thymoma.
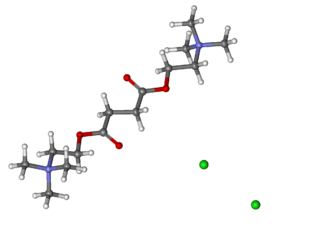
Suxamethonium chloride, [Scoline, Sucostrin] also known as suxamethonium or succinylcholine, or simply sux by medical abbreviation, is a medication used to cause short-term paralysis as part of general anesthesia. This is done to help with tracheal intubation or electroconvulsive therapy. It is administered by injection, either into a vein or into a muscle. When used in a vein, onset of action is generally within one minute and effects last for up to 10 minutes.
A neuromuscular junction is a chemical synapse between a motor neuron and a muscle fiber.
Muscle fatigue is when muscles that were initially generating a normal amount of force, then experience a declining ability to generate force. It can be a result of vigorous exercise, but abnormal fatigue may be caused by barriers to or interference with the different stages of muscle contraction. There are two main causes of muscle fatigue: the limitations of a nerve’s ability to generate a sustained signal ; and the reduced ability of the muscle fiber to contract.

Electromyography (EMG) is a technique for evaluating and recording the electrical activity produced by skeletal muscles. EMG is performed using an instrument called an electromyograph to produce a record called an electromyogram. An electromyograph detects the electric potential generated by muscle cells when these cells are electrically or neurologically activated. The signals can be analyzed to detect abnormalities, activation level, or recruitment order, or to analyze the biomechanics of human or animal movement. Needle EMG is an electrodiagnostic medicine technique commonly used by neurologists. Surface EMG is a non-medical procedure used to assess muscle activation by several professionals, including physiotherapists, kinesiologists and biomedical engineers. In computer science, EMG is also used as middleware in gesture recognition towards allowing the input of physical action to a computer as a form of human-computer interaction.

A nerve conduction study (NCS) is a medical diagnostic test commonly used to evaluate the function, especially the ability of electrical conduction, of the motor and sensory nerves of the human body. These tests may be performed by medical specialists such as clinical neurophysiologists, physical therapists, physiatrists, and neurologists who subspecialize in electrodiagnostic medicine. In the United States, neurologists and physiatrists receive training in electrodiagnostic medicine as part of residency training and in some cases acquire additional expertise during a fellowship in clinical neurophysiology, electrodiagnostic medicine, or neuromuscular medicine. Outside the US, clinical neurophysiologists learn needle EMG and NCS testing.
Myotonia congenita is a congenital neuromuscular channelopathy that affects skeletal muscles. It is a genetic disorder. The hallmark of the disease is the failure of initiated contraction to terminate, often referred to as delayed relaxation of the muscles (myotonia) and rigidity. Symptoms include delayed relaxation of the muscles after voluntary contraction (myotonia), and may also include stiffness, hypertrophy (enlargement), transient weakness in some forms of the disorder, severe masseter spasm, and cramping. The condition is sometimes referred to as fainting goat syndrome, as it is responsible for the eponymous 'fainting' seen in fainting goats when presented with a sudden stimulus. Of note, myotonia congenita has no association with malignant hyperthermia (MH).

Hypokalemic periodic paralysis (hypoKPP), also known as familial hypokalemic periodic paralysis (FHPP), is a rare, autosomal dominant channelopathy characterized by muscle weakness or paralysis when there is a fall in potassium levels in the blood. In individuals with this mutation, attacks sometimes begin in adolescence and most commonly occur with individual triggers such as rest after strenuous exercise, high carbohydrate meals, meals with high sodium content, sudden changes in temperature, and even excitement, noise, flashing lights, cold temperatures and stress. Weakness may be mild and limited to certain muscle groups, or more severe full-body paralysis. During an attack, reflexes may be decreased or absent. Attacks may last for a few hours or persist for several days. Recovery is usually sudden when it occurs, due to release of potassium from swollen muscles as they recover. Some patients may fall into an abortive attack or develop chronic muscle weakness later in life.

In neuroscience, nerve conduction velocity (CV) is the speed at which an electrochemical impulse propagates down a neural pathway. Conduction velocities are affected by a wide array of factors, which include age, sex, and various medical conditions. Studies allow for better diagnoses of various neuropathies, especially demyelinating diseases as these conditions result in reduced or non-existent conduction velocities. CV is an important aspect of nerve conduction studies.

Centronuclear myopathies (CNM) are a group of congenital myopathies where cell nuclei are abnormally located in the center of muscle cells instead of their normal location at the periphery.
The triceps reflex, a deep tendon reflex, is a reflex that elicits involuntary contraction of the triceps brachii muscle. It is sensed and transmitted by the radial nerve. The reflex is tested as part of the neurological examination to assess the sensory and motor pathways within the C7 and C8 spinal nerves.
Motor unit number estimation (MUNE) is a technique that uses electromyography to estimate the number of motor units in a muscle.
Critical illness polyneuropathy (CIP) and critical illness myopathy (CIM) are overlapping syndromes of diffuse, symmetric, flaccid muscle weakness occurring in critically ill patients and involving all extremities and the diaphragm with relative sparing of the cranial nerves. CIP and CIM have similar symptoms and presentations and are often distinguished largely on the basis of specialized electrophysiologic testing or muscle and nerve biopsy. The causes of CIP and CIM are unknown, though they are thought to be a possible neurological manifestation of systemic inflammatory response syndrome. Corticosteroids and neuromuscular blocking agents, which are widely used in intensive care, may contribute to the development of CIP and CIM, as may elevations in blood sugar, which frequently occur in critically ill patients.

Inflammatory myopathy, also known as idiopathic inflammatory myopathy (IIM), is disease featuring muscle weakness, inflammation of muscles (myositis), and in some types, muscle pain. The cause of much inflammatory myopathy is unknown (idiopathic), and such cases are classified according to their symptoms and signs, electromyography, MRI, and laboratory findings. It can also be associated with underlying cancer. The main classes of idiopathic inflammatory myopathy are polymyositis (PM), dermatomyositis (DM), inclusion-body myositis (IBM), immune-mediated necrotising myopathy (IMNM), and focal autoimmune myositis.
Repetitive nerve stimulation is a variant of the nerve conduction study where electrical stimulation is delivered to a motor nerve repeatedly several times per second. By observing the change in the muscle electrical response (CMAP) after several stimulations, a physician can assess for the presence of a neuromuscular junction disease, and differentiate between presynaptic and postsynaptic conditions. The test was first described by German neurologist Friedrich Jolly in 1895, and is also known as Jolly's test.
Acquired non-inflammatory myopathy (ANIM) is a neuromuscular disorder primarily affecting skeletal muscle, most commonly in the limbs of humans, resulting in a weakness or dysfunction in the muscle. A myopathy refers to a problem or abnormality with the myofibrils, which compose muscle tissue. In general, non-inflammatory myopathies are a grouping of muscular diseases not induced by an autoimmune-mediated inflammatory pathway. These muscular diseases usually arise from a pathology within the muscle tissue itself rather than the nerves innervating that tissue. ANIM has a wide spectrum of causes which include drugs and toxins, nutritional imbalances, acquired metabolic dysfunctions such as an acquired defect in protein structure, and infections.
Electromyoneurography (EMNG) is the combined use of electromyography and electroneurography This technique allows for the measurement of a peripheral nerve's conduction velocity upon stimulation (electroneurography) alongside electrical recording of muscular activity (electromyography). Their combined use proves to be clinically relevant by allowing for both the source and location of a particular neuromuscular disease to be known, and for more accurate diagnoses.