Related Research Articles

Health care, health-care, or healthcare is the maintenance or improvement of health via the prevention, diagnosis, treatment, recovery, or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals in allied health fields. Physicians and physician associates are a part of these health professionals. Dentistry, pharmacy, midwifery, nursing, medicine, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training and other health professions are all part of health care. It includes work done in providing primary care, secondary care, and tertiary care, as well as in public health.

The American Medical Association (AMA), founded in 1847 and incorporated in 1897, is the largest association of physicians—both MDs and DOs—and medical students in the United States.

The Canada Health Act (CHA) is a piece of Government of Canada legislation, adopted in 1984, which specifies the conditions and criteria with which the provincial and territorial health insurance programs must conform in order to receive federal transfer payments under the Canada Health Transfer. These criteria require universal coverage of all insured services.
The British Medical Association (BMA) is the professional association and registered trade union for doctors in the United Kingdom. The association does not regulate or certify doctors, a responsibility which lies with the General Medical Council. The association's headquarters are located in BMA House, Tavistock Square, London. Additionally, the association has national offices in Cardiff, Belfast, and Edinburgh, a European office in Brussels and a number of offices in English regions. The BMA has a range of representative and scientific committees and is recognised by National Health Service (NHS) employers as sole contract negotiators for doctors.
Single-payer healthcare is a type of universal healthcare that covers the costs of essential healthcare for all residents, with costs covered by a single public system.

School nursing, a specialized practice of public health nursing, protects and promotes student health, facilitates normal development, and advances academic success. School nurses, grounded in ethical and evidence-based practice, are the leaders that bridge health care and education, provide care coordination, advocate for quality student-centered care, and collaborate to design systems that allow individuals and communities to develop their full potentials.
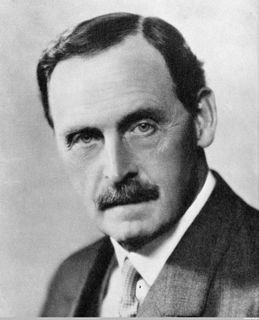
Bertrand Edward Dawson, 1st Viscount Dawson of Penn, was a physician to the British Royal Family and President of the Royal College of Physicians from 1931 to 1937.

NHS Scotland, sometimes styled NHSScotland, is the publicly funded healthcare system in Scotland, and one of the four systems which make up the National Health Service in the United Kingdom. It operates fourteen territorial NHS boards across Scotland, seven special non-geographic health boards and NHS Health Scotland.

The name National Health Service (NHS) is used to refer to the three public health services of England, Scotland and Wales, individually or collectively. Northern Ireland is known as 'Health and Social Care' to promote its dual integration of health and social services.
This Act of Parliament established for the first time in the United Kingdom a Minister of Health.

The National Health Service Act 1946 came into effect on 5 July 1948 and created the National Health Service in England and Wales. Though the title 'National Health Service' implies a single health service for the United Kingdom, in reality one NHS was created for England and Wales accountable to the Secretary of State for Health, with a separate NHS created for Scotland accountable to the Secretary of State for Scotland by the passage of the National Health Service (Scotland) Act 1947. Similar health services in Northern Ireland were created by the Northern Ireland Parliament through the Health Services Act 1948.
The Australian College of Rural and Remote Medicine (ACRRM) is one of the two Australian Medical Council (AMC) accredited general practice colleges in Australia. The College sets and upholds standards for best practice provision of rural and remote medical care. It provides training and certification, and professional development for rural general practice. It also provides advocacy and support for current and prospective rural doctors.

Australia has a highly developed health care structure, though because of its vast size, services are not evenly distributed. Health care is delivered in Australia by both government and private companies which are often covered by Medicare. Health care in Australia is largely funded by the government at national, state and local governmental levels, as well as by private health insurance; but the cost of health care is also borne by not-for-profit organisations, with a significant cost being borne by individual patients or by charity. Some services are provided by volunteers, especially remote and mental health services.
The Highlands and Islands Medical Service (HIMS) provided state funded healthcare to a population covering half of Scotland's landmass from its launch in 1913 until the creation of Scotland's National Health Service (NHS) in 1948. Though treatment was not free, unlike NHS Scotland which succeeded it, fees were set at minimal levels and people could still get treated even if they were unable to pay.
Hong Kong's medical infrastructure consists of a mixed medical economy, with 12 private hospitals and 43 public hospitals. Hong Kong has high standards of medical practice. It has contributed to the development of liver transplantation, being the first in the world to carry out an adult to adult live donor liver transplant in 1993. Both public and private hospitals in Hong Kong have partnered with the Australian Council on Healthcare Standards (ACHS) for international healthcare accreditation. There are also polyclinics that offer primary care services, including dentistry.

The Ministry of Health (MoH) is the government ministry of Ghana that is responsible for the health of Ghana. It is involved in providing public health services, managing Ghana's healthcare industry, and building Ghana's hospitals and medical education system.

A healthcare center, health center, or community health center is one of a network of clinics staffed by a group of general practitioners and nurses providing healthcare services to people in a certain area. Typical services covered are family practice and dental care, but some clinics have expanded greatly and can include internal medicine, pediatric, women’s care, family planning, pharmacy, optometry, laboratory testing, and more. In countries with universal healthcare, most people use the healthcare centers. In countries without universal healthcare, the clients include the uninsured, underinsured, low-income or those living in areas where little access to primary health care is available. In the Central and East Europe, bigger health centres are commonly called policlinics.
The Report of the Highlands and Islands Medical Service Committee or the Dewar Report was published in 1912 and named after its chair, Sir John Dewar. The report presented a vivid description of the social landscape of the time and highlighted the desperate state of medical provision to the population, particularly in the rural areas of the Highlands and Islands of Scotland. The report recommended setting up a new, centrally planned provision of care that within 20 years transformed medical services to the area. This organisation, the Highlands and Islands Medical Service was widely cited in the Cathcart Report and acted as a working blueprint for the NHS in Scotland. The report is written in clear language and many of its findings continue to have relevance to how medical services are planned and financed in Scotland and beyond.
The Patient Protection and Affordable Care Act (PPACA) is divided into 10 titles and contains provisions that became effective immediately, 90 days after enactment, and six months after enactment, as well as provisions phased in through to 2020. Below are some of the key provisions of the ACA. For simplicity, the amendments in the Health Care and Education Reconciliation Act of 2010 are integrated into this timeline.
The Consultative Council on National Health Insurance was established under the Ministry of Health Act 1919 along with the National Health Insurance Joint Committee.
References
- ↑ Rivett, Geoffrey. "The Development of the London Hospital System, 1823 - 2015". National Health Service History. Retrieved 10 November 2016.
- ↑ "Interim Report on the Future Provision of Medical and Allied Services 1920". Socialist Health Association. HMSO. Retrieved 10 November 2016.
- ↑ "Records of the National Health Insurance Joint Committee, Commissions, and Consultative Council". The National Archives. Retrieved 10 November 2016.