Related Research Articles
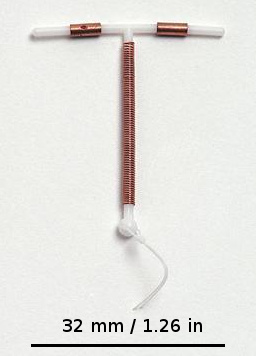
A copper intrauterine device (IUD), also known as an intrauterine coil or copper coil or non-hormonal IUD, is a type of intrauterine device which contains copper. It is used for birth control and emergency contraception within five days of unprotected sex. It is one of the most effective forms of birth control with a one-year failure rate around 0.7%. The device is placed in the uterus and lasts up to twelve years. It may be used by women of all ages regardless of whether or not they have had children. Following removal, fertility quickly returns.

Emergency contraception (EC) is a birth control measure, used after sexual intercourse to prevent pregnancy.
Sterilization is any of a number of medical methods of permanent birth control that intentionally leaves a person unable to reproduce. Sterilization methods include both surgical and non-surgical options for both males and females. Sterilization procedures are intended to be permanent; reversal is generally difficult.

Tubal ligation is a surgical procedure for female sterilization in which the fallopian tubes are permanently blocked, clipped or removed. This prevents the fertilization of eggs by sperm and thus the implantation of a fertilized egg. Tubal ligation is considered a permanent method of sterilization and birth control.

Family planning is the consideration of the number of children a person wishes to have, including the choice to have no children, and the age at which they wish to have them. Things that may play a role on family planning decisions include marital situation, career or work considerations, financial situations. If sexually active, family planning may involve the use of contraception and other techniques to control the timing of reproduction.

A hormonal intrauterine device (IUD), also known as an intrauterine system (IUS) with progestogen and sold under the brand name Mirena among others, is an intrauterine device that releases a progestogenic hormonal agent such as levonorgestrel into the uterus. It is used for birth control, heavy menstrual periods, and to prevent excessive build of the lining of the uterus in those on estrogen replacement therapy. It is one of the most effective forms of birth control with a one-year failure rate around 0.2%. The device is placed in the uterus and lasts three to eight years. Fertility often returns quickly following removal.

Hormonal contraception refers to birth control methods that act on the endocrine system. Almost all methods are composed of steroid hormones, although in India one selective estrogen receptor modulator is marketed as a contraceptive. The original hormonal method—the combined oral contraceptive pill—was first marketed as a contraceptive in 1960. In the ensuing decades, many other delivery methods have been developed, although the oral and injectable methods are by far the most popular. Hormonal contraception is highly effective: when taken on the prescribed schedule, users of steroid hormone methods experience pregnancy rates of less than 1% per year. Perfect-use pregnancy rates for most hormonal contraceptives are usually around the 0.3% rate or less. Currently available methods can only be used by women; the development of a male hormonal contraceptive is an active research area.

There are many methods of birth control that vary in requirements, side effects, and effectiveness. As the technology, education, and awareness about contraception has evolved, new contraception methods have been theorized and put in application. Although no method of birth control is ideal for every user, some methods remain more effective, affordable or intrusive than others. Outlined here are the different types of barrier methods, hormonal methods, various methods including spermicides, emergency contraceptives, and surgical methods and a comparison between them.
Contraceptive security is an individual's ability to reliably choose, obtain, and use quality contraceptives for family planning and the prevention of sexually transmitted diseases. The term refers primarily to efforts undertaken in low and middle-income countries to ensure contraceptive availability as an integral part of family planning programs. Even though there is a consistent increase in the use of contraceptives in low, middle, and high-income countries, the actual contraceptive use varies in different regions of the world. The World Health Organization recognizes the importance of contraception and describes all choices regarding family planning as human rights. Subsidized products, particularly condoms and oral contraceptives, may be provided to increase accessibility for low-income people. Measures taken to provide contraceptive security may include strengthening contraceptive supply chains, forming contraceptive security committees, product quality assurance, promoting supportive policy environments, and examining financing options.
Long-acting reversible contraceptives (LARC) are methods of birth control that provide effective contraception for an extended period without requiring user action. They include hormonal and non-hormonal intrauterine devices (IUDs), and subdermal hormonal contraceptive implants. They are the most effective reversible methods of contraception because their efficacy is not reliant on patient compliance. The failure rates of IUDs and implants is less than 1% per year.

Birth control, also known as contraception, anticonception, and fertility control, is the use of methods or devices to prevent unintended pregnancy. Birth control has been used since ancient times, but effective and safe methods of birth control only became available in the 20th century. Planning, making available, and using human birth control is called family planning. Some cultures limit or discourage access to birth control because they consider it to be morally, religiously, or politically undesirable.
Unintended pregnancies are pregnancies that are mistimed or unwanted at the time of conception, also known as unplanned pregnancies.

Family planning in India is based on efforts largely sponsored by the Indian government. From 1965 to 2009, contraceptive usage has more than tripled and the fertility rate has more than halved, but the national fertility rate in absolute numbers remains high, causing concern for long-term population growth. India adds up to 1,000,000 people to its population every 20 days. Extensive family planning has become a priority in an effort to curb the projected population of two billion by the end of the twenty-first century.

Even though there is considerable demand for family planning in Pakistan, the adoption of family planning has been hampered by government neglect, lack of services and misconceptions. Demographics play a large role in Pakistan's development and security since the change from military rule to civilian leadership. Challenges to Pakistani's well-being, opportunities for education and employment, and access to health care are escalated due to the country's continuously-growing population. It was estimated in 2005 that Pakistan's population totaled 151 million; a number which grows 1.9 percent annually, equaling a 2.9 million population growth per year. Though Pakistan's fertility rates still exceed those of neighboring South Asian countries with a total fertility rate at 4.1 and contraception use is lower than 35 percent, approximately one-fourth of Pakistani women wish to either delay the birth of their next child or end childbearing altogether.
Reproductive coercion is a collection of behaviors that interfere with decision-making related to reproductive health. These behaviors are meant to maintain power and control related to reproductive health by a current, former, or hopeful intimate or romantic partner, but they can also be perpetrated by parents or in-laws. Coercive behaviors infringe on individuals' reproductive rights and reduce their reproductive autonomy.
Abortion in Cuba is legal and available upon request, which is rare in Latin America because of widespread Catholic influence.

Access to safe and adequate sexual and reproductive healthcare constitutes part of the Universal Declaration of Human Rights, as upheld by the United Nations.

Globally approximately 45% of those who are married and able to have children use contraception. As of 2007, IUDs were used by about 17% of women of child bearing age in developing countries and 9% in developed countries or more than 180 million women worldwide. Avoiding sex when fertile is used by about 3.6% of women of childbearing age, with usage as high as 20% in areas of South America. As of 2005, 12% of couples are using a male form of contraception with rates of up to 30% in the developed world.
Women's reproductive health in the United States refers to the set of physical, mental, and social issues related to the health of women in the United States. It includes the rights of women in the United States to adequate sexual health, available contraception methods, and treatment for sexually transmitted diseases. The prevalence of women's health issues in American culture is inspired by second-wave feminism in the United States. As a result of this movement, women of the United States began to question the largely male-dominated health care system and demanded a right to information on issues regarding their physiology and anatomy. The U.S. government has made significant strides to propose solutions, like creating the Women's Health Initiative through the Office of Research on Women's Health in 1991. However, many issues still exist related to the accessibility of reproductive healthcare as well as the stigma and controversy attached to sexual health, contraception, and sexually transmitted diseases.
Family planning in Bangladesh is carried out by government agencies and supported by non-government organisations. The Directorate General of Family Planning is the government agency responsible for family planning in Bangladesh. Marie Stopes Bangladesh is an international NGO that provides family planning services in Bangladesh.
References
- 1 2 National Institute of Population Research and Training (NIPORT); Mitra and Associates; ICF International (2016). Bangladesh Demographic and Health Survey 2014 (PDF) (Report). NIPORT, Mitra and Associates, and ICF International. p. 74. Retrieved 2019-02-03.
- 1 2 3 4 Huda, Fauzia Akhter; Robertson, Yolande; Chowdhuri, Sabiha; Sarker, Bidhan Krishna; Reichenbach, Laura; Somrongthong, Ratana (2017). "Contraceptive practices among married women of reproductive age in Bangladesh: a review of the evidence". Reproductive Health. 14 (1): 69. doi: 10.1186/s12978-017-0333-2 . ISSN 1742-4755. PMC 5461624 . PMID 28587619.
- ↑ "Contraceptive prevalence rate (CPR) — MEASURE Evaluation". www.measureevaluation.org. Retrieved 2020-05-10.
- ↑ Kamal, Mostafa; Islam, Aynul (2011). "Prevalence and socioeconomic correlates of unintented pregnancy among women in rural Bangladesh". Salud Pública de México. 53 (2): 108–115. doi: 10.1590/S0036-36342011000200003 . ISSN 0036-3634.
- 1 2 Saha, Unnati Rani; Bairagi, Radheshyam (2007). "Inconsistencies in the Relationship Between Contraceptive Use and Fertility in Bangladesh" (PDF). International Family Planning Perspectives. 33 (1): 31–37. doi: 10.1363/3303107 . ISSN 0190-3187.
- 1 2 Al Kibria, Gulam Muhammed; Hossen, Shakir; Barsha, Rifath Ara Alam; Sharmeen, Atia; Paul, Sujit Kumar; Uddin, S. M. Iftekhar (2016). "Factors affecting contraceptive use among married women of reproductive age in Bangladesh" (PDF). Journal of Molecular Studies and Medicine Research. 2 (1): 70–79. doi:10.18801/jmsmr.020116.09.
- ↑ Islam, Sabina; Islam, Mohammad Amirul; Padmadas, Sabu S. (2010). "High Fertility Regions in Bangladesh: A Marriage Cohort Analysis" (PDF). Journal of Biosocial Science. 42 (6): 705–719. doi:10.1017/S0021932010000428. ISSN 0021-9320.