Related Research Articles

Angina, also known as angina pectoris, is chest pain or pressure, usually caused by insufficient blood flow to the heart muscle (myocardium). It is most commonly a symptom of coronary artery disease.
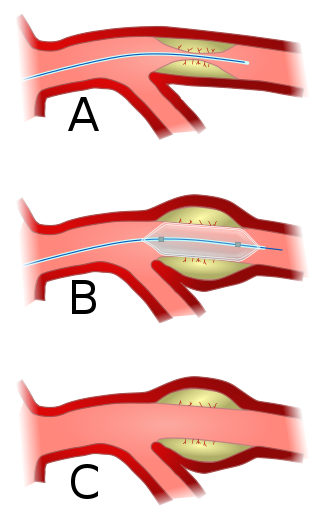
Angioplasty, also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis.

Aortic stenosis is the narrowing of the exit of the left ventricle of the heart, such that problems result. It may occur at the aortic valve as well as above and below this level. It typically gets worse over time. Symptoms often come on gradually with a decreased ability to exercise often occurring first. If heart failure, loss of consciousness, or heart related chest pain occur due to AS the outcomes are worse. Loss of consciousness typically occurs with standing or exercising. Signs of heart failure include shortness of breath especially when lying down, at night, or with exercise, and swelling of the legs. Thickening of the valve without causing obstruction is known as aortic sclerosis.

Coronary artery bypass surgery, also known as coronary artery bypass graft, is a surgical procedure to treat coronary artery disease (CAD), the buildup of plaques in the arteries of the heart. It can relieve chest pain caused by CAD, slow the progression of CAD, and increase life expectancy. It aims to bypass narrowings in heart arteries by using arteries or veins harvested from other parts of the body, thus restoring adequate blood supply to the previously ischemic heart.

Echocardiography, also known as cardiac ultrasound, is the use of ultrasound to examine the heart. It is a type of medical imaging, using standard ultrasound or Doppler ultrasound. The visual image formed using this technique is called an echocardiogram, a cardiac echo, or simply an echo.

A coronary catheterization is a minimally invasive procedure to access the coronary circulation and blood filled chambers of the heart using a catheter. It is performed for both diagnostic and interventional (treatment) purposes.

A cardiac stress test is a cardiological examination that evaluates the cardiovascular system's response to external stress within a controlled clinical setting. This stress response can be induced through physical exercise or intravenous pharmacological stimulation of heart rate.
Intravascular ultrasound (IVUS) or intravascular echocardiography is a medical imaging methodology using a specially designed catheter with a miniaturized ultrasound probe attached to the distal end of the catheter. The proximal end of the catheter is attached to computerized ultrasound equipment. It allows the application of ultrasound technology, such as piezoelectric transducer or CMUT, to see from inside blood vessels out through the surrounding blood column, visualizing the endothelium of blood vessels.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.

Renal artery stenosis (RAS) is the narrowing of one or both of the renal arteries, most often caused by atherosclerosis or fibromuscular dysplasia. This narrowing of the renal artery can impede blood flow to the target kidney, resulting in renovascular hypertension – a secondary type of high blood pressure. Possible complications of renal artery stenosis are chronic kidney disease and coronary artery disease.
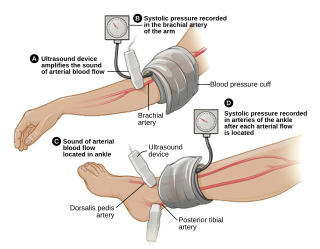
The ankle-brachial pressure index (ABPI) or ankle-brachial index (ABI) is the ratio of the blood pressure at the ankle to the blood pressure in the upper arm (brachium). Compared to the arm, lower blood pressure in the leg suggests blocked arteries due to peripheral artery disease (PAD). The ABPI is calculated by dividing the systolic blood pressure at the ankle by the systolic blood pressure in the arm.

Valvular heart disease is any cardiovascular disease process involving one or more of the four valves of the heart. These conditions occur largely as a consequence of aging, but may also be the result of congenital (inborn) abnormalities or specific disease or physiologic processes including rheumatic heart disease and pregnancy.
Coronary artery anomalies are variations of the coronary circulation, affecting <1% of the general population. Symptoms include chest pain, shortness of breath and syncope, although cardiac arrest may be the first clinical presentation. Several varieties are identified, with a different potential to cause sudden cardiac death.
Fractional flow reserve (FFR) is a diagnostic technique used in coronary catheterization. FFR measures pressure differences across a coronary artery stenosis to determine the likelihood that the stenosis impedes oxygen delivery to the heart muscle.
The following outline is provided as an overview of and topical guide to cardiology, the branch of medicine dealing with disorders of the human heart. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease and electrophysiology. Physicians who specialize in cardiology are called cardiologists.

Anomalous left coronary artery from the pulmonary artery is a rare congenital anomaly occurring in approximately 1 in 300,000 liveborn children. The diagnosis comprises between 0.24 and 0.46% of all cases of congenital heart disease. The anomalous left coronary artery (LCA) usually arises from the pulmonary artery instead of the aortic sinus. In fetal life, the high pressure in the pulmonic artery and the fetal shunts enable oxygen-rich blood to flow in the LCA. By the time of birth, the pressure will decrease in the pulmonic artery and the child will have a postnatal circulation. The myocardium which is supplied by the LCA, will therefore be dependent on collateral blood flow from the other coronary arteries, mainly the RCA. Because the pressure in RCA exceeds the pressure in LCA a collateral circulation will increase. This situation ultimately can lead to blood flowing from the RCA into the LCA retrograde and into the pulmonary artery, thus forming a left-to-right shunt.

A myocardial bridge (MB) is a [[congenital common heart anomaly] in which one of the coronary arteries tunnels through the heart muscle itself (myocardium). In most of the people, the coronary arteries rest on top of the heart muscle and feed blood down into smaller vessels which then take blood into the heart muscle itself. However, if a band of muscle forms around one of the coronary arteries during the fetal stage of development, then a myocardial bridge is formed – a "bridge" of heart muscle over the artery. Each time the heart squeezes to pump blood, the band of muscle exerts pressure and it is very rarely constricts the artery, reducing blood flow to the heart. This is present from birth. It is important to note that even a very thin ex. <1 mm and/or short ex. 20 mm MB can cause significant symptoms(This is not proven).MBs can range from a few mm in length to 10 cm or more. The overall prevalence of myocardial bridge is 19%, although its prevalence found by autopsy is much higher (42%).A myocardial bridge is a usually harmless condition in which one or more of the coronary arteries goes through the heart muscle instead of lying on its surface. Most bridges don’t seem to cause symptoms. However, some people with myocardial bridges can experience angina, or chest pain.

Spontaneous coronary artery dissection (SCAD) is an uncommon but potentially lethal condition in which one of the coronary arteries that supply the heart, spontaneously develops a blood collection, or hematoma, within the artery wall due to a tear in the wall. SCAD is one of the arterial dissections that can occur.

Coronary perfusion pressure (CPP) refers to the pressure gradient that drives coronary blood pressure. The heart's function is to perfuse blood to the body; however, the heart's own myocardium must, itself, be supplied for its own muscle function. The heart is supplied by coronary vessels, and therefore CPP is the blood pressure within those vessels. If pressures are too low in the coronary vasculature, then the myocardium risks ischemia with subsequent myocardial infarction or cardiogenic shock.
Cardiac imaging refers to minimally invasive imaging of the heart using ultrasound, magnetic resonance imaging (MRI), computed tomography (CT), or nuclear medicine (NM) imaging with PET or SPECT. These cardiac techniques are otherwise referred to as echocardiography, Cardiac MRI, Cardiac CT, Cardiac PET and Cardiac SPECT including myocardial perfusion imaging.
References
- 1 2 Radó, Julia; Forster, Tamás (2001). "The significance of coronary flow reserve in chest pain syndromes" (PDF). Echo in Context. Archived from the original (PDF) on 11 June 2012.
- ↑ Klabunde, Richard E. (28 March 2014). "Critical Stenosis". Cardiovascular Physiology Concepts. Archived from the original on 30 June 2014.
- 1 2 Holdright, DR; Lindsay, DC; Clarke, D; Fox, K; et al. (1993). "Coronary flow reserve in patients with chest pain and normal coronary arteries". British Heart Journal. 70 (6): 513–9. doi:10.1136/hrt.70.6.513. PMC 1025381 . PMID 8280515.
- ↑ Serruys, PW; Zijlstra, F; Laarman, GJ; Reiber, HH; et al. (August 1989). "A comparison of two methods to measure coronary flow reserve in the setting of coronary angioplasty: Intracoronary blood flow velocity measurements with a Doppler catheter, and digital subtraction cineangiography". European Heart Journal. 10 (8): 725–36. doi:10.1093/oxfordjournals.eurheartj.a059557. hdl: 1765/4331 . PMID 2529120.
- 1 2 Dimitrow, PP; Krzanowski, M; Undas, A (2005). "Reduced coronary flow reserve in Anderson-Fabry disease measured by transthoracic Doppler echocardiography". Cardiovascular Ultrasound. 3: 11. doi: 10.1186/1476-7120-3-11 . PMC 1097744 . PMID 15857518.
- ↑ Galderisi, M; D'Errico, A (2008). "Beta-blockers and coronary flow reserve: The importance of a vasodilatory action". Drugs. 68 (5): 579–90. doi:10.2165/00003495-200868050-00002. PMID 18370439. S2CID 218465204.
- ↑ Zehetgruber, M; Mundigler, G; Christ, G; Mörtl, D; Probst, P; Baumgartner, H; Maurer, G; Siostrzonek, P (1995). "Estimation of coronary flow reserve by transesophageal coronary sinus Doppler measurements in patients with syndrome X and patients with significant left coronary artery disease". Journal of the American College of Cardiology. 25 (5): 1039–45. doi: 10.1016/0735-1097(94)00544-Z . PMID 7897114.
- ↑ Hess, OM; McGillem, MJ; DeBoe, SF; Pinto, IM; et al. (1990). "Determination of coronary flow reserve by parametric imaging". Circulation. 82 (4): 1438–48. doi: 10.1161/01.CIR.82.4.1438 . PMID 2144799.