Related Research Articles

Heinrich Hermann Robert Koch was a German physician and microbiologist. As the discoverer of the specific causative agents of deadly infectious diseases including tuberculosis, cholera and anthrax, he is regarded as one of the main founders of modern bacteriology. As such he is popularly nicknamed the father of microbiology, and as the father of medical bacteriology. His discovery of the anthrax bacterium in 1876 is considered as the birth of modern bacteriology. Koch used his discoveries to establish that germs "could cause a specific disease" and directly provided proofs for that germ theory of diseases, therefore creating the scientific basis of public health, saving millions of lives.

Tuberculosis (TB) is an infectious disease usually caused by Mycobacterium tuberculosis (MTB) bacteria. Tuberculosis generally affects the lungs, but it can also affect other parts of the body. Most infections show no symptoms, in which case it is known as latent tuberculosis. Around 10% of latent infections progress to active disease which, if left untreated, kill about half of those affected. Typical symptoms of active TB are chronic cough with blood-containing mucus, fever, night sweats, and weight loss. It was historically referred to as consumption due to the weight loss associated with the disease. Infection of other organs can cause a wide range of symptoms.

An infection is the invasion of tissues by pathogens, their multiplication, and the reaction of host tissues to the infectious agent and the toxins they produce. An infectious disease, also known as a transmissible disease or communicable disease, is an illness resulting from an infection.

The Mantoux test or Mendel–Mantoux test is a tool for screening for tuberculosis (TB) and for tuberculosis diagnosis. It is one of the major tuberculin skin tests used around the world, largely replacing multiple-puncture tests such as the tine test. The Heaf test, a form of tine test, was used until 2005 in the UK, when it was replaced by the Mantoux test. The Mantoux test is endorsed by the American Thoracic Society and Centers for Disease Control and Prevention. It was also used in the USSR and is now prevalent in most of the post-Soviet states, although Soviet mantoux produced many false positives due to children's allergic reaction.
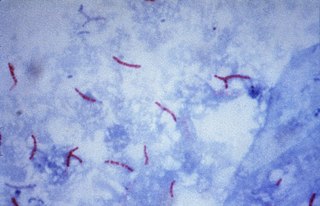
Mycobacterium tuberculosis, also known as Koch's bacillus, is a species of pathogenic bacteria in the family Mycobacteriaceae and the causative agent of tuberculosis. First discovered in 1882 by Robert Koch, M. tuberculosis has an unusual, waxy coating on its cell surface primarily due to the presence of mycolic acid. This coating makes the cells impervious to Gram staining, and as a result, M. tuberculosis can appear weakly Gram-positive. Acid-fast stains such as Ziehl–Neelsen, or fluorescent stains such as auramine are used instead to identify M. tuberculosis with a microscope. The physiology of M. tuberculosis is highly aerobic and requires high levels of oxygen. Primarily a pathogen of the mammalian respiratory system, it infects the lungs. The most frequently used diagnostic methods for tuberculosis are the tuberculin skin test, acid-fast stain, culture, and polymerase chain reaction.

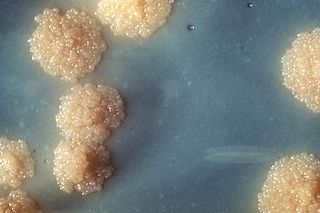
Mycobacterium is a genus of over 190 species in the phylum Actinomycetota, assigned its own family, Mycobacteriaceae. This genus includes pathogens known to cause serious diseases in mammals, including tuberculosis and leprosy in humans. The Greek prefix myco- means 'fungus', alluding to this genus' mold-like colony surfaces. Since this genus has cell walls with a waxy lipid-rich outer layer that contains high concentrations of mycolic acid, acid-fast staining is used to emphasize their resistance to acids, compared to other cell types.

A granuloma is an aggregation of macrophages that forms in response to chronic inflammation. This occurs when the immune system attempts to isolate foreign substances that it is otherwise unable to eliminate. Such substances include infectious organisms including bacteria and fungi, as well as other materials such as foreign objects, keratin, and suture fragments.

An asymptomatic carrier is a person or other organism that has become infected with a pathogen, but shows no signs or symptoms.

Mycobacterium bovis is a slow-growing aerobic bacterium and the causative agent of tuberculosis in cattle. It is related to Mycobacterium tuberculosis, the bacterium which causes tuberculosis in humans. M. bovis can jump the species barrier and cause tuberculosis-like infection in humans and other mammals.

The rifamycins are a group of antibiotics that are synthesized either naturally by the bacterium Amycolatopsis rifamycinica or artificially. They are a subclass of the larger family of ansamycins. Rifamycins are particularly effective against mycobacteria, and are therefore used to treat tuberculosis, leprosy, and mycobacterium avium complex (MAC) infections.

Tuberculosis management describes the techniques and procedures utilized for treating tuberculosis (TB).

Miliary tuberculosis is a form of tuberculosis that is characterized by a wide dissemination into the human body and by the tiny size of the lesions (1–5 mm). Its name comes from a distinctive pattern seen on a chest radiograph of many tiny spots distributed throughout the lung fields with the appearance similar to millet seeds—thus the term "miliary" tuberculosis. Miliary TB may infect any number of organs, including the lungs, liver, and spleen. Miliary tuberculosis is present in about 2% of all reported cases of tuberculosis and accounts for up to 20% of all extra-pulmonary tuberculosis cases.
Following infection with HIV-1, the rate of clinical disease progression varies between individuals. Factors such as host susceptibility, genetics and immune function, health care and co-infections as well as viral genetic variability may affect the rate of progression to the point of needing to take medication in order not to develop AIDS.

Mycobacterium avium-intracellulare infection (MAI) is an atypical mycobacterial infection, i.e. one with nontuberculous mycobacteria or NTM, caused by Mycobacterium avium complex (MAC), which is made of two Mycobacterium species, M. avium and M. intracellulare. This infection causes respiratory illness in birds, pigs, and humans, especially in immunocompromised people. In the later stages of AIDS, it can be very severe. It usually first presents as a persistent cough. It is typically treated with a series of three antibiotics for a period of at least six months.
Latent tuberculosis (LTB), also called latent tuberculosis infection (LTBI) is when a person is infected with Mycobacterium tuberculosis, but does not have active tuberculosis (TB). Active tuberculosis can be contagious while latent tuberculosis is not, and it is therefore not possible to get TB from someone with latent tuberculosis. The main risk is that approximately 10% of these people will go on to develop active tuberculosis. This is particularly true, and there is added risk, in particular situations such as medication that suppresses the immune system or advancing age.

A mycobacteriophage is a member of a group of bacteriophages known to have mycobacteria as host bacterial species. While originally isolated from the bacterial species Mycobacterium smegmatis and Mycobacterium tuberculosis, the causative agent of tuberculosis, more than 4,200 mycobacteriophage have since been isolated from various environmental and clinical sources. 2,042 have been completely sequenced. Mycobacteriophages have served as examples of viral lysogeny and of the divergent morphology and genetic arrangement characteristic of many phage types.
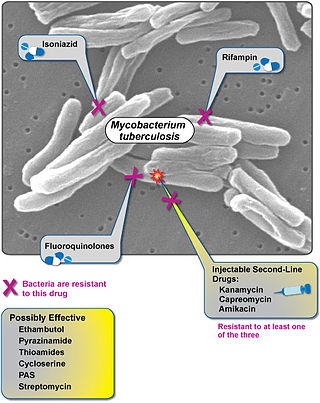
Extensively drug-resistant tuberculosis (XDR-TB) is a form of tuberculosis caused by bacteria that are resistant to some of the most effective anti-TB drugs. XDR-TB strains have arisen after the mismanagement of individuals with multidrug-resistant TB (MDR-TB).
Multidrug-resistant tuberculosis (MDR-TB) is a form of tuberculosis (TB) infection caused by bacteria that are resistant to treatment with at least two of the most powerful first-line anti-TB medications (drugs): isoniazid and rifampin. Some forms of TB are also resistant to second-line medications, and are called extensively drug-resistant TB (XDR-TB).

Tuberculosis in India is a major health problem, causing about 220,000 deaths every year. In 2020, the Indian government made statements to eliminate tuberculosis from the country by 2025 through its National TB Elimination Program. Interventions in this program include major investment in health care, providing supplemental nutrition credit through the Nikshay Poshan Yojana, organizing a national epidemiological survey for tuberculosis, and organizing a national campaign to tie together the Indian government and private health infrastructure for the goal of eliminating the disease.
The co-epidemic of tuberculosis (TB) and human immunodeficiency virus (HIV) is one of the major global health challenges in the present time. The World Health Organization (WHO) reports 9.2 million new cases of TB in 2006 of whom 7.7% were HIV-infected. Tuberculosis is the most common contagious infection in HIV-Immunocompromised patients leading to death. These diseases act in combination as HIV drives a decline in immunity while tuberculosis progresses due to defective immune status. This condition becomes more severe in case of multi-drug (MDRTB) and extensively drug resistant TB (XDRTB), which are difficult to treat and contribute to increased mortality. Tuberculosis can occur at any stage of HIV infection. The risk and severity of tuberculosis increases soon after infection with HIV. A study on gold miners of South Africa revealed that the risk of TB was doubled during the first year after HIV seroconversion. Although tuberculosis can be a relatively early manifestation of HIV infection, it is important to note that the risk of tuberculosis progresses as the CD4 cell count decreases along with the progression of HIV infection. The risk of TB generally remains high in HIV-infected patients, remaining above the background risk of the general population even with effective immune reconstitution and high CD4 cell counts with antiretroviral therapy.
References
- ↑ Brust, J. (6 Jan 2011). "Culture Conversion Among HIV Co-Infected Multidrug-Resistant Tuberculosis Patients in Tugela Ferry, South Africa". PLOS ONE . 6 (1): e15841. Bibcode:2011PLoSO...615841B. doi: 10.1371/journal.pone.0015841 . PMC 3017058 . PMID 21253585.
- ↑ Su, W.J. (1 Jun 2010). "Role of 2-month sputum smears in predicting culture conversion in pulmonary tuberculosis". European Respiratory Journal. 37 (2): 376–383. doi: 10.1183/09031936.00007410 . PMID 20516049 . Retrieved 16 September 2014.