Emergency contraception (EC) is a birth control measure, used after sexual intercourse to prevent pregnancy.

Fertility awareness (FA) refers to a set of practices used to determine the fertile and infertile phases of a woman's menstrual cycle. Fertility awareness methods may be used to avoid pregnancy, to achieve pregnancy, or as a way to monitor gynecological health.

The combined oral contraceptive pill (COCP), often referred to as the birth control pill or colloquially as "the pill", is a type of birth control that is designed to be taken orally by women. It is the oral form of combined hormonal contraception. The pill contains two important hormones: a progestin and estrogen. When taken correctly, it alters the menstrual cycle to eliminate ovulation and prevent pregnancy.
The Pearl Index, also called the Pearl rate, is the most common technique used in clinical trials for reporting the effectiveness of a birth control method. It is a very approximate measure of the number of unintended pregnancies in 100 woman-years of exposure that is simple to calculate, but has a number of methodological deficiencies.
Calendar-based methods are various methods of estimating a woman's likelihood of fertility, based on a record of the length of previous menstrual cycles. Various methods are known as the Knaus–Ogino method and the rhythm method. The standard days method is also considered a calendar-based method, because when using it, a woman tracks the days of her menstrual cycle without observing her physical fertility signs. The standard days method is based on a fixed formula taking into consideration the timing of ovulation, the functional life of the sperm and the ovum, and the resulting likelihood of pregnancy on particular days of the menstrual cycle. These methods may be used to achieve pregnancy by timing unprotected intercourse for days identified as fertile, or to avoid pregnancy by avoiding unprotected intercourse during fertile days.
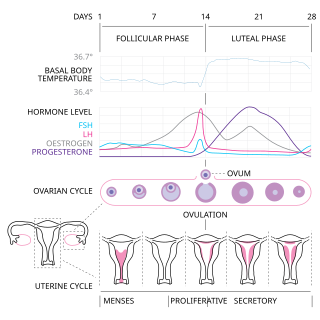
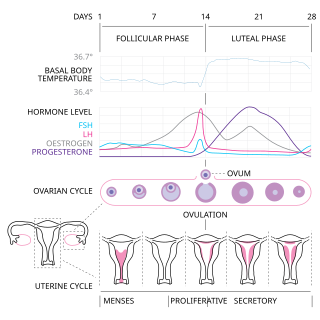
The menstrual cycle is a series of natural changes in hormone production and the structures of the uterus and ovaries of the female reproductive system that makes pregnancy possible. The ovarian cycle controls the production and release of eggs and the cyclic release of estrogen and progesterone. The uterine cycle governs the preparation and maintenance of the lining of the uterus (womb) to receive an embryo. These cycles are concurrent and coordinated, normally last between 21 and 35 days, with a median length of 28 days. Menarche usually occurs around the age of 12 years; menstrual cycles continue for about 30–45 years.

Ovulation is an important part of the menstrual cycle in female vertebrates where the egg cells are released from the ovaries as part of the ovarian cycle. In human females ovulation typically occurs near the midpoint in the menstrual cycle and after the follicular phase. Ovulation is stimulated by an increase in luteinizing hormone (LH). The ovarian follicles rupture and release the secondary oocyte ovarian cells.

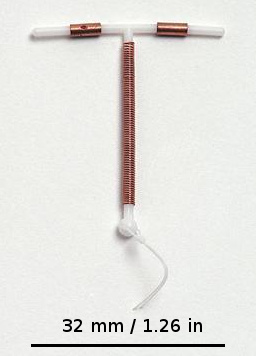
A hormonal intrauterine device (IUD), also known as an intrauterine system (IUS) with progestogen and sold under the brand name Mirena among others, is an intrauterine device that releases a progestogenic hormonal agent such as levonorgestrel into the uterus. It is used for birth control, heavy menstrual periods, and to prevent excessive build of the lining of the uterus in those on estrogen replacement therapy. It is one of the most effective forms of birth control with a one-year failure rate around 0.2%. The device is placed in the uterus and lasts three to eight years. Fertility often returns quickly following removal.
Natural family planning (NFP) comprises the family planning methods approved by the Catholic Church and some Protestant denominations for both achieving and postponing or avoiding pregnancy. In accordance with the Church's teachings regarding sexual behavior, NFP excludes the use of other methods of birth control, which it refers to as "artificial contraception".
Basal body temperature is the lowest body temperature attained during rest. It is usually estimated by a temperature measurement immediately after awakening and before any physical activity has been undertaken. This will lead to a somewhat higher value than the true BBT.

Lactational amenorrhea, also called postpartum infertility, is the temporary postnatal infertility that occurs when a woman is amenorrheic and fully breastfeeding.

Hormonal contraception refers to birth control methods that act on the endocrine system. Almost all methods are composed of steroid hormones, although in India one selective estrogen receptor modulator is marketed as a contraceptive. The original hormonal method—the combined oral contraceptive pill—was first marketed as a contraceptive in 1960. In the ensuing decades, many other delivery methods have been developed, although the oral and injectable methods are by far the most popular. Hormonal contraception is highly effective: when taken on the prescribed schedule, users of steroid hormone methods experience pregnancy rates of less than 1% per year. Perfect-use pregnancy rates for most hormonal contraceptives are usually around the 0.3% rate or less. Currently available methods can only be used by women; the development of a male hormonal contraceptive is an active research area.

There are many methods of birth control that vary in requirements, side effects, and effectiveness. As the technology, education, and awareness about contraception has evolved, new contraception methods have been theorized and put in application. Although no method of birth control is ideal for every user, some methods remain more effective, affordable or intrusive than others. Outlined here are the different types of barrier methods, hormonal methods, various methods including spermicides, emergency contraceptives, and surgical methods and a comparison between them.
Long-acting reversible contraceptives (LARC) are methods of birth control that provide effective contraception for an extended period without requiring user action. They include hormonal and non-hormonal intrauterine devices (IUDs) and subdermal hormonal contraceptive implants. They are the most effective reversible methods of contraception because their efficacy is not reliant on patient compliance. The failure rates of IUDs and implants is less than 1% per year.

Birth control, also known as contraception, anticonception, and fertility control, is the use of methods or devices to prevent pregnancy. Birth control has been used since ancient times, but effective and safe methods of birth control only became available in the 20th century. Planning, making available, and using human birth control is called family planning. Some cultures limit or discourage access to birth control because they consider it to be morally, religiously, or politically undesirable.
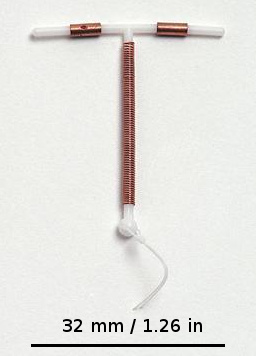
An intrauterine device (IUD), also known as an intrauterine contraceptive device or coil, is a small, often T-shaped birth control device that is inserted into the uterus to prevent pregnancy. IUDs are a form of long-acting reversible contraception (LARC).
James Boyer Brown MSc (NZ) PhD (Edin) DSc (Edin) FRACOG, Professor Emeritus, Department of Obstetrics and Gynaecology, University of Melbourne.
Women's reproductive health in the United States refers to the set of physical, mental, and social issues related to the health of women in the United States. It includes the rights of women in the United States to adequate sexual health, available contraception methods, and treatment for sexually transmitted diseases. The prevalence of women's health issues in American culture is inspired by second-wave feminism in the United States. As a result of this movement, women of the United States began to question the largely male-dominated health care system and demanded a right to information on issues regarding their physiology and anatomy. The U.S. government has made significant strides to propose solutions, like creating the Women's Health Initiative through the Office of Research on Women's Health in 1991. However, many issues still exist related to the accessibility of reproductive healthcare as well as the stigma and controversy attached to sexual health, contraception, and sexually transmitted diseases.
Natural Cycles is a mobile app designed to help women track their fertility. The app predicts the days on which a woman is fertile and may be used for planning pregnancy and contraception. It was developed by scientist Elina Berglund, who founded the company with her husband, Raoul Scherwitzl.
The TwoDay Method is a Fertility awareness method used to either avoid or achieve pregnancy.