Antinuclear antibodies are autoantibodies that bind to contents of the cell nucleus. In normal individuals, the immune system produces antibodies to foreign proteins (antigens) but not to human proteins (autoantigens). In some cases, antibodies to human antigens are produced; these are known as autoantibodies.
Spondyloarthritis (SpA), also known as spondyloarthropathy, is a collection of clinical syndromes that are connected by genetic predisposition and clinical manifestations. The best-known clinical subtypes are enteropathic arthritis (EA), psoriatic arthritis (PsA), ankylosing spondylitis (AS), and reactive arthritis (ReA). Spondyloarthritis typically presents with inflammatory back pain and asymmetrical arthritis, primarily affecting the lower limbs, and enthesitis, inflammation at bone-adhering ligaments, tendons, or joint capsules.

Rheumatism /ˈruməˌtɪzəm/ or rheumatic disorders are conditions causing chronic, often intermittent pain affecting the joints or connective tissue. Rheumatism does not designate any specific disorder, but covers at least 200 different conditions, including arthritis and "non-articular rheumatism", also known as "regional pain syndrome" or "soft tissue rheumatism". There is a close overlap between the term soft tissue disorder and rheumatism. Sometimes the term "soft tissue rheumatic disorders" is used to describe these conditions.

Psoriatic arthritis (PsA) is a long-term inflammatory arthritis that occurs in people affected by the autoimmune disease psoriasis. The classic feature of psoriatic arthritis is swelling of entire fingers and toes with a sausage-like appearance. This often happens in association with damage to the nails such as small depressions in the nail (pitting), thickening of the nails, and detachment of the nail from the nailbed. Skin damage consistent with psoriasis frequently occur before the onset of psoriatic arthritis but psoriatic arthritis can precede the rash in 15% of affected individuals. It is classified as a type of seronegative spondyloarthropathy.
Connective tissue disease, also known as connective tissue disorder, or collagen vascular diseases, refers to any disorder that affects the connective tissue. The body's structures are held together by connective tissues, consisting of two distinct proteins: elastin and collagen. Tendons, ligaments, skin, cartilage, bone, and blood vessels are all made of collagen. Skin and ligaments contain elastin. The proteins and the body's surrounding tissues may suffer damage when these connective tissues become inflamed.
Mixed connective tissue disease (MCTD) is a systemic autoimmune disease that shares characteristics with at least two other systemic autoimmune diseases, including systemic sclerosis (Ssc), systemic lupus erythematosus (SLE), polymyositis/dermatomyositis (PM/DM), and rheumatoid arthritis. The idea behind the "mixed" disease is that this specific autoantibody is also present in other autoimmune diseases such as systemic lupus erythematosus, polymyositis, scleroderma, etc. MCTD was characterized as an individual disease in 1972 by Sharp et al., and the term was introduced by Leroy in 1980.
Biological response modifiers (BRMs) are substances that modify immune responses. They can be endogenous or exogenous, and they can either enhance an immune response or suppress it. Some of these substances arouse the body's response to an infection, and others can keep the response from becoming excessive. Thus they serve as immunomodulators in immunotherapy, which can be helpful in treating cancer and in treating autoimmune diseases, such as some kinds of arthritis and dermatitis. Most BRMs are biopharmaceuticals (biologics), including monoclonal antibodies, interleukin 2, interferons, and various types of colony-stimulating factors. "Immunotherapy makes use of BRMs to enhance the activity of the immune system to increase the body's natural defense mechanisms against cancer", whereas BRMs for rheumatoid arthritis aim to reduce inflammation.
Anti-topoisomerase antibodies (ATA) are autoantibodies directed against topoisomerase and found in several diseases, most importantly scleroderma. Diseases with ATA are autoimmune disease because they react with self-proteins. They are also referred to as anti-DNA topoisomerase I antibody.
Michael D. Lockshin is an American professor and medical researcher. He is known for his work as a researcher of autoimmune diseases, with focus on antiphospholipid syndrome and lupus. He is Professor Emeritus of Medicine and the Director Emeritus of the Barbara Volcker Center for Women and Rheumatic Disease at Hospital for Special Surgery. He retired from HSS on January 31, 2023.

Lupus, formally called systemic lupus erythematosus (SLE), is an autoimmune disease in which the body's immune system mistakenly attacks healthy tissue in many parts of the body. Symptoms vary among people and may be mild to severe. Common symptoms include painful and swollen joints, fever, chest pain, hair loss, mouth ulcers, swollen lymph nodes, feeling tired, and a red rash which is most commonly on the face. Often there are periods of illness, called flares, and periods of remission during which there are few symptoms. Children up to 18 years old develop a more severe form of SLE termed childhood-onset systemic lupus erythematosus.
Lupus headache is a proposed, specific headache disorder in patients with systemic lupus erythematosus (SLE). Research shows that headache is a symptom commonly described by SLE patients —57% in one meta-analysis, ranging in different studies from 33% to 78%; of which migraine 31.7% and tension-type headache 23.5%. The existence of a special lupus headache is contested, although few high-quality studies are available to form definitive conclusions.
Blisibimod is a selective antagonist of B-cell activating factor, being developed by Anthera Pharmaceuticals as a treatment for systemic lupus erythematosus. It is currently under active investigation in clinical trials.

Anthera Pharmaceuticals, Inc. is an American biopharmaceutical company focused on developing and commercializing products to treat serious conditions associated with cystic fibrosis, inflammation and autoimmune diseases. Liprotamase (Sollpura), Anthera's leading drug candidate which is being developed for exocrine pancreatic insufficiency (EPI) is currently in Phase 3 clinical trials, and A-623 (Blisibimod) for the treatment of IgA nephropathy is currently in Phase 2 clinical trial.
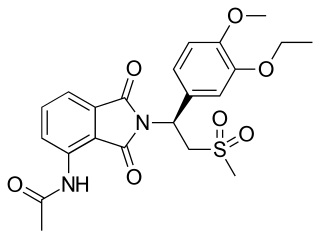
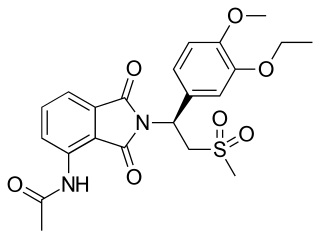
Apremilast, sold under the brand name Otezla among others, is a medication for the treatment of certain types of psoriasis and psoriatic arthritis. The drug acts as a selective inhibitor of the enzyme phosphodiesterase 4 (PDE4). It is taken by mouth.

Lupus vasculitis is one of the secondary vasculitides that occurs in approximately 50% of patients with systemic lupus erythematosus (SLE).
Neuropsychiatric systemic lupus erythematosus or NPSLE refers to the neurological and psychiatric manifestations of systemic lupus erythematosus. SLE is a disease in which the immune system attacks the body's own cells and tissues. It can affect various organs or systems of the body. It is estimated that over half of people with SLE have neuropsychiatric involvement.

Robert George Lahita is an American physician, internist and rheumatologist, best known for his research into systemic lupus erythematosus. and other autoimmune diseases. He is the author of more than 16 books and 150 scientific publications in the field of autoimmunity and immuno-endocrinology and a media consultant on health-related issues. He currently serves as Director of the Institute of Autoimmune and Rheumatic Diseases at St. Joseph's Healthcare System, specializing in autoimmunity, rheumatology, and treatment of diseases of joints, muscle, bones and tendons including arthritis, back pain, muscle strains, common athletic injuries and collagen diseases.

Lars Klareskog is a Swedish physician, immunologist, and rheumatologist, known for research into the genetics of autoimmune diseases such as rheumatoid arthritis (RA).
Childhood-onset systemic lupus erythematosus, also termed juvenile-onset systemic lupus erythematosus, juvenile systemic lupus erythematosus, and pediatric systemic lupus erythematosus, is a form of the chronic inflammatory and autoimmune disease, systemic lupus erythematosus, that develops in individuals up to 18 years old. Early-onset systemic lupus erythematosus is often used to designate a subset of cSLE patients who are up to 5 years old. Children with early-onset SLE tend to have a more severe form of cSLE than children who develop cSLE after 5 years of age.