Coitus interruptus, also known as withdrawal, pulling out, or the pull-out method, is a method of birth control in which a man, during sexual intercourse, withdraws his penis from a woman's vagina prior to ejaculation and then directs his ejaculate (semen) away from the vagina in an effort to avoid insemination.

Intrauterine device (IUD) with copper, also known as intrauterine coil, is a type of intrauterine device which contains copper. It is used for birth control and emergency contraception within five days of unprotected sex. It is one of the most effective forms of birth control with a one-year failure rate around 0.7%. The device is placed in the uterus and lasts up to twelve years. It may be used by women of all ages regardless of whether or not they have had children. Following removal, fertility quickly returns.

Emergency contraception (EC) are birth control measures that may be used after sexual intercourse to prevent pregnancy.

Fertility awareness (FA) refers to a set of practices used to determine the fertile and infertile phases of a woman's menstrual cycle. Fertility awareness methods may be used to avoid pregnancy, to achieve pregnancy, or as a way to monitor gynecological health.

The combined oral contraceptive pill (COCP), often referred to as the birth control pill or colloquially as "the pill", is a type of birth control that is designed to be taken orally by women. It includes a combination of an estrogen and a progestogen. When taken correctly, it alters the menstrual cycle to eliminate ovulation and prevent pregnancy.
The Pearl Index, also called the Pearl rate, is the most common technique used in clinical trials for reporting the effectiveness of a birth control method.
Calendar-based methods are various methods of estimating a woman's likelihood of fertility, based on a record of the length of previous menstrual cycles. Various methods are known as the Knaus–Ogino method and the rhythm method. The standard days method is also considered a calendar-based method, because when using it, a woman tracks the days of her menstrual cycle without observing her physical fertility signs. The standard days method is based on a fixed formula taking into consideration the timing of ovulation, the functional life of the sperm and the ovum, and the resulting likelihood of pregnancy on particular days of the menstrual cycle. These methods may be used to achieve pregnancy by timing unprotected intercourse for days identified as fertile, or to avoid pregnancy by avoiding unprotected intercourse during fertile days.

Tubal ligation is a surgical procedure for female sterilization in which the fallopian tubes are permanently blocked or removed. This prevents the fertilization of eggs by sperm and thus the implantation of a fertilized egg. Tubal ligation is considered a permanent method of sterilization and birth control.

The diaphragm is a barrier method of birth control. It is moderately effective, with a one-year failure rate of around 12% with typical use. It is placed over the cervix with spermicide before sex and left in place for at least six hours after sex. Fitting by a healthcare provider is generally required.
Spermicide is a contraceptive substance that destroys sperm, inserted vaginally prior to intercourse to prevent pregnancy. As a contraceptive, spermicide may be used alone. However, the pregnancy rate experienced by couples using only spermicide is higher than that of couples using other methods. Usually, spermicides are combined with contraceptive barrier methods such as diaphragms, condoms, cervical caps, and sponges. Combined methods are believed to result in lower pregnancy rates than either method alone.

Levonorgestrel is a hormonal medication which is used in a number of birth control methods. It is combined with an estrogen to make combination birth control pills. As an emergency birth control, sold under the brand name Plan B among others, it is useful within 72 hours. This should not be confused with EllaOne which can be effective within 120 hours of unprotected sex. The more time that has passed since sex, the less effective the medication becomes, and it does not work after pregnancy (implantation) has occurred. It decreases the chances of pregnancy by 57 to 93%. In an intrauterine device (IUD), such as Mirena among others, it is effective for the long-term prevention of pregnancy. A levonorgestrel-releasing implant is also available in some countries.

Vaginal rings are polymeric drug delivery devices designed to provide controlled release of drugs for intravaginal administration over extended periods of time. The ring is inserted into the vagina and provides contraception protection. Vaginal rings come in one size that fits most women.

Lactational amenorrhea, also called postpartum infertility, is the temporary postnatal infertility that occurs when a woman is amenorrheic and fully breastfeeding.
Hormonal contraception refers to birth control methods that act on the endocrine system. Almost all methods are composed of steroid hormones, although in India one selective estrogen receptor modulator is marketed as a contraceptive. The original hormonal method—the combined oral contraceptive pill—was first marketed as a contraceptive in 1960. In the ensuing decades many other delivery methods have been developed, although the oral and injectable methods are by far the most popular. Hormonal contraception is highly effective: when taken on the prescribed schedule, users of steroid hormone methods experience pregnancy rates of less than 1% per year. Perfect-use pregnancy rates for most hormonal contraceptives are usually around the 0.3% rate or less. Currently available methods can only be used by women; the development of a male hormonal contraceptive is an active research area.
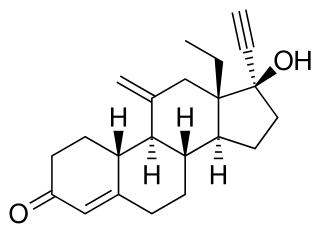
Etonogestrel is a medication which is used as a means of birth control for women. It is available as an implant placed under the skin of the upper arm under the brand names Nexplanon and Implanon, and in combination with ethinylestradiol, an estrogen, as a vaginal ring under the brand names NuvaRing and Circlet. Etonogestrel is effective as a means of birth control within 8 hours of insertion and lasts at least three or four years with some data showing effectiveness for five years. Following removal, fertility quickly returns.

There are many different methods of birth control, which vary in what is required of the user, side effects, and effectiveness. It is also important to note that not each type of birth control is ideal for each user. Outlined here are the different types of barrier methods, spermicides, or coitus interruptus that must be used at or before every act of intercourse. Immediate contraception, like physical barriers, include diaphragms, caps, the contraceptive sponge, and female condoms may be placed several hours before intercourse begins. The female condom should be removed immediately after intercourse, and before arising.[1] Some other female barrier methods must be left in place for several hours after sex. Depending on the form of spermicide used, they may be applied several minutes to an hour before intercourse begins. Additionally, the male condom should be applied when the penis is erect so that it is properly applied prior to intercourse.

Birth control, also known as contraception, anticonception, and fertility control, is a method or device used to prevent pregnancy. Birth control has been used since ancient times, but effective and safe methods of birth control only became available in the 20th century. Planning, making available, and using birth control is called family planning. Some cultures limit or discourage access to birth control because they consider it to be morally, religiously, or politically undesirable.
Unintended pregnancies are pregnancies that are mistimed, unplanned or unwanted at the time of conception.

An intrauterine device (IUD), also known as intrauterine contraceptive device or coil, is a small, often T-shaped birth control device that is inserted into the uterus to prevent pregnancy. IUDs are one form of long-acting reversible birth control (LARC). One study found that female family planning providers choose LARC methods more often (41.7%) than the general public (12.1%). Among birth control methods, IUDs, along with other contraceptive implants, result in the greatest satisfaction among users.
Hanna Klaus is an Obstetrics and gynaecology physician, a member of the Medical Mission Sisters, and best known as founder of the TeenSTAR adolescent sex education program.