The Hippocratic Oath is an oath of ethics historically taken by physicians. It is one of the most widely known of Greek medical texts. In its original form, it requires a new physician to swear, by a number of healing gods, to uphold specific ethical standards. The oath is the earliest expression of medical ethics in the Western world, establishing several principles of medical ethics which remain of paramount significance today. These include the principles of medical confidentiality and non-maleficence. As the seminal articulation of certain principles that continue to guide and inform medical practice, the ancient text is of more than historic and symbolic value. It is enshrined in the legal statutes of various jurisdictions, such that violations of the oath may carry criminal or other liability beyond the oath's symbolic nature.

Informed consent is a principle in medical ethics, medical law and media studies, that a patient must have sufficient information and understanding before making decisions about their medical care. Pertinent information may include risks and benefits of treatments, alternative treatments, the patient's role in treatment, and their right to refuse treatment. In most systems, healthcare providers have a legal and ethical responsibility to ensure that a patient's consent is informed. This principle applies more broadly than healthcare intervention, for example to conduct research and to disclose a person's medical information.

Emergency medicine is the medical speciality concerned with the care of illnesses or injuries requiring immediate medical attention. Emergency physicians specialize in providing care for unscheduled and undifferentiated patients of all ages. As first-line providers, in coordination with emergency medical services, they are primarily responsible for initiating resuscitation and stabilization and performing the initial investigations and interventions necessary to diagnose and treat illnesses or injuries in the acute phase. Emergency medical physicians generally practice in hospital emergency departments, pre-hospital settings via emergency medical services, and intensive care units. Still, they may also work in primary care settings such as urgent care clinics.
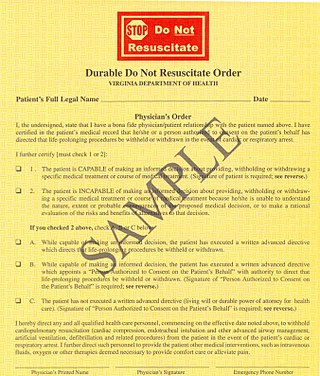
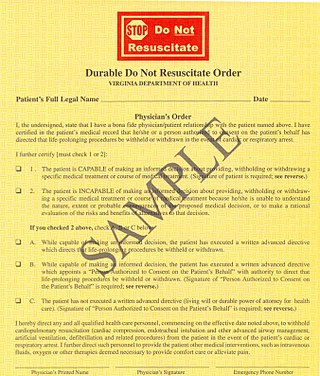
A do-not-resuscitate order (DNR), also known as Do Not Attempt Resuscitation (DNAR), Do Not Attempt Cardiopulmonary Resuscitation (DNACPR), no code or allow natural death, is a medical order, written or oral depending on the jurisdiction, indicating that a person should not receive cardiopulmonary resuscitation (CPR) if that person's heart stops beating. Sometimes these decisions and the relevant documents also encompass decisions around other critical or life-prolonging medical interventions. The legal status and processes surrounding DNR orders vary in different polities. Most commonly, the order is placed by a physician based on a combination of medical judgement and patient involvement.
Medical ethics is an applied branch of ethics which analyzes the practice of clinical medicine and related scientific research. Medical ethics is based on a set of values that professionals can refer to in the case of any confusion or conflict. These values include the respect for autonomy, non-maleficence, beneficence, and justice. Such tenets may allow doctors, care providers, and families to create a treatment plan and work towards the same common goal. These four values are not ranked in order of importance or relevance and they all encompass values pertaining to medical ethics. However, a conflict may arise leading to the need for hierarchy in an ethical system, such that some moral elements overrule others with the purpose of applying the best moral judgement to a difficult medical situation. Medical ethics is particularly relevant in decisions regarding involuntary treatment and involuntary commitment.

Geriatrics, or geriatric medicine, is a medical specialty focused on providing care for the unique health needs of the elderly. The term geriatrics originates from the Greek γέρων geron meaning "old man", and ιατρός iatros meaning "healer". It aims to promote health by preventing, diagnosing and treating disease in older adults. There is no defined age at which patients may be under the care of a geriatrician, or geriatric physician, a physician who specializes in the care of older people. Rather, this decision is guided by individual patient need and the caregiving structures available to them. This care may benefit those who are managing multiple chronic conditions or experiencing significant age-related complications that threaten quality of daily life. Geriatric care may be indicated if caregiving responsibilities become increasingly stressful or medically complex for family and caregivers to manage independently.

Human subject research is systematic, scientific investigation that can be either interventional or observational and involves human beings as research subjects, commonly known as test subjects. Human subject research can be either medical (clinical) research or non-medical research. Systematic investigation incorporates both the collection and analysis of data in order to answer a specific question. Medical human subject research often involves analysis of biological specimens, epidemiological and behavioral studies and medical chart review studies. On the other hand, human subject research in the social sciences often involves surveys which consist of questions to a particular group of people. Survey methodology includes questionnaires, interviews, and focus groups.
A Physician Assistant or Physician Associate (PA) is a type of healthcare professional. While these job titles are used internationally, there is significant variation in training and scope of practice from country to country, and sometimes between smaller jurisdictions such as states or provinces. Depending on location, PAs practice semi-autonomously under the supervision of a physician, or autonomously perform a subset of medical services classically provided by physicians.
A medical error is a preventable adverse effect of care ("iatrogenesis"), whether or not it is evident or harmful to the patient. This might include an inaccurate or incomplete diagnosis or treatment of a disease, injury, syndrome, behavior, infection, or other ailment.
Pharmaceutical marketing is a branch of marketing science and practice focused on the communication, differential positioning and commercialization of pharmaceutical products, like specialist drugs, biotech drugs and over-the-counter drugs. By extension, this definition is sometimes also used for marketing practices applied to nutraceuticals and medical devices.
Medical torture describes the involvement of, or sometimes instigation by, medical personnel in acts of torture, either to judge what victims can endure, to apply treatments which will enhance torture, or as torturers in their own right. Medical torture overlaps with medical interrogation if it involves the use of professional medical expertise to facilitate interrogation or corporal punishment, in the conduct of torturous human experimentation or in providing professional medical sanction and approval for the torture of prisoners. Medical torture also covers torturous scientific experimentation upon unwilling human subjects.
password Professionalization or professionalisation is a social process by which any trade or occupation transforms itself into a true "profession of the highest integrity and competence." The definition of what constitutes a profession is often contested. Professionalization tends to result in establishing acceptable qualifications, one or more professional associations to recommend best practice and to oversee the conduct of members of the profession, and some degree of demarcation of the qualified from unqualified amateurs. It is also likely to create "occupational closure", closing the profession to entry from outsiders, amateurs and the unqualified.

Sleep medicine is a medical specialty or subspecialty devoted to the diagnosis and therapy of sleep disturbances and disorders. From the middle of the 20th century, research has provided increasing knowledge of, and answered many questions about, sleep–wake functioning. The rapidly evolving field has become a recognized medical subspecialty in some countries. Dental sleep medicine also qualifies for board certification in some countries. Properly organized, minimum 12-month, postgraduate training programs are still being defined in the United States. In some countries, the sleep researchers and the physicians who treat patients may be the same people.
The doctor–patient relationship is a central part of health care and the practice of medicine. A doctor–patient relationship is formed when a doctor attends to a patient's medical needs and is usually through consent. This relationship is built on trust, respect, communication, and a common understanding of both the doctor and patients' sides. The trust aspect of this relationship goes is mutual: the doctor trusts the patient to reveal any information that may be relevant to the case, and in turn, the patient trusts the doctor to respect their privacy and not disclose this information to outside parties.
Fee splitting is the practice of sharing fees with professional colleagues, such as physicians or lawyers, in return for being sent referrals.
Participation of medical professionals in American executions is a controversial topic, due to its moral and legal implications. The practice is proscribed by the American Medical Association, as defined in its Code of Medical Ethics. The American Society of Anesthesiologists endorses this position, stating that lethal injections "can never conform to the science, art and practice of anesthesiology".
Clinical peer review, also known as medical peer review is the process by which health care professionals, including those in nursing and pharmacy, evaluate each other's clinical performance. A discipline-specific process may be referenced accordingly.
Healthgrades Marketplace, LLC, known as Healthgrades, is a US company that provides information about physicians, hospitals, and healthcare providers. Healthgrades is part of RVO Health, a partnership between Red Ventures and Optum, part of UnitedHealth Group. Healthgrades has amassed information on over three million U.S. health care providers. The company was founded by Kerry Hicks, David Hicks, Peter Fatianow, John Neal, and Sarah Lochran, and is based in Denver, Colorado. Jeff Hallock serves as RVO Health's CEO. According to USA Today, Healthgrades is the first comprehensive physician rating and comparison database. The application is part of a trend in health technology in the United States towards consumer-driven healthcare.
A medical scribe is an allied health paraprofessional who specializes in charting physician-patient encounters in real time, such as during medical examinations. They also locate information and patients for physicians and complete forms needed for patient care. Depending on which area of practice the scribe works in, the position may also be called clinical scribe, ER scribe or ED scribe, or just scribe. A scribe is trained in health information management and the use of health information technology to support it. A scribe can work on-site or remotely from a HIPAA-secure facility. Medical scribes who work at an off-site location are known as virtual medical scribes.
Various organizations of practicing chiropractors have outlined formal codes of professional ethics. Actual practice has revealed a wide range of behaviors which may or may not conform to these standards.
Jacob DeLaRosa. The Disruptive Physician, How to Manage the Consequences of Being You Misner & Monroe, New York 2017