The respiratory tract is the subdivision of the respiratory system involved with the process of respiration in mammals. The respiratory tract is lined with respiratory epithelium as respiratory mucosa.

Bronchiectasis is a disease in which there is permanent enlargement of parts of the airways of the lung. Symptoms typically include a chronic cough with mucus production. Other symptoms include shortness of breath, coughing up blood, and chest pain. Wheezing and nail clubbing may also occur. Those with the disease often get lung infections.

Bronchospasm or a bronchial spasm is a sudden constriction of the muscles in the walls of the bronchioles. It is caused by the release (degranulation) of substances from mast cells or basophils under the influence of anaphylatoxins. It causes difficulty in breathing which ranges from mild to severe.

Non-invasive ventilation (NIV) is the use of breathing support administered through a face mask, nasal mask, or a helmet. Air, usually with added oxygen, is given through the mask under positive pressure; generally the amount of pressure is alternated depending on whether someone is breathing in or out. It is termed "non-invasive" because it is delivered with a mask that is tightly fitted to the face or around the head, but without a need for tracheal intubation. While there are similarities with regard to the interface, NIV is not the same as continuous positive airway pressure (CPAP), which applies a single level of positive airway pressure throughout the whole respiratory cycle; CPAP does not deliver ventilation but is occasionally used in conditions also treated with NIV.

Bronchoconstriction is the constriction of the airways in the lungs due to the tightening of surrounding smooth muscle, with consequent coughing, wheezing, and shortness of breath.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.
Occupational lung diseases are work-related, lung conditions that have been caused or made worse by the materials a person is exposed to within the workplace. It includes a broad group of diseases, including occupational asthma, industrial bronchitis, chronic obstructive pulmonary disease (COPD), bronchiolitis obliterans, inhalation injury, interstitial lung diseases, infections, lung cancer and mesothelioma. These diseases can be caused directly or due to immunological response to an exposure to a variety of dusts, chemicals, proteins or organisms.
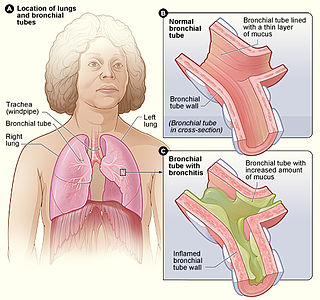
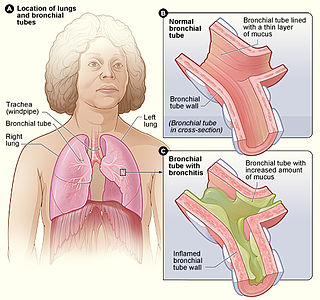
Bronchitis is inflammation of the bronchi in the lungs that causes coughing. Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi. Symptoms include coughing up sputum, wheezing, shortness of breath, and chest pain. Bronchitis can be acute or chronic.

Obstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself. It is generally characterized by inflamed and easily collapsible airways, obstruction to airflow, problems exhaling, and frequent medical clinic visits and hospitalizations. Types of obstructive lung disease include; asthma, bronchiectasis, bronchitis and chronic obstructive pulmonary disease (COPD). Although COPD shares similar characteristics with all other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms, and reversibility of airway obstruction. Cystic fibrosis is also sometimes included in obstructive pulmonary disease.

Pulmonary function testing (PFT) is a complete evaluation of the respiratory system including patient history, physical examinations, and tests of pulmonary function. The primary purpose of pulmonary function testing is to identify the severity of pulmonary impairment. Pulmonary function testing has diagnostic and therapeutic roles and helps clinicians answer some general questions about patients with lung disease. PFTs are normally performed by a pulmonary function technician, respiratory therapist, respiratory physiologist, physiotherapist, pulmonologist, or general practitioner.

Diffuse panbronchiolitis (DPB) is an inflammatory lung disease of unknown cause. It is a severe, progressive form of bronchiolitis, an inflammatory condition of the bronchioles. The term diffuse signifies that lesions appear throughout both lungs, while panbronchiolitis refers to inflammation found in all layers of the respiratory bronchioles. DPB causes severe inflammation and nodule-like lesions of terminal bronchioles, chronic sinusitis, and intense coughing with large amounts of sputum production.
Bronchial hyperresponsiveness is a state characterised by easily triggered bronchospasm.
Pulmonary rehabilitation, also known as respiratory rehabilitation, is an important part of the management and health maintenance of people with chronic respiratory disease who remain symptomatic or continue to have decreased function despite standard medical treatment. It is a broad therapeutic concept. It is defined by the American Thoracic Society and the European Respiratory Society as an evidence-based, multidisciplinary, and comprehensive intervention for patients with chronic respiratory diseases who are symptomatic and often have decreased daily life activities. In general, pulmonary rehabilitation refers to a series of services that are administered to patients of respiratory disease and their families, typically to attempt to improve the quality of life for the patient. Pulmonary rehabilitation may be carried out in a variety of settings, depending on the patient's needs, and may or may not include pharmacologic intervention.

An acute exacerbation of chronic obstructive pulmonary disease, or acute exacerbations of chronic bronchitis (AECB), is a sudden worsening of chronic obstructive pulmonary disease (COPD) symptoms including shortness of breath, quantity and color of phlegm that typically lasts for several days.

Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. The main symptoms of COPD include shortness of breath and a cough, which may or may not produce mucus. COPD progressively worsens, with everyday activities such as walking or dressing becoming difficult. While COPD is incurable, it is preventable and treatable.
Ravi Kalhan is the director of the Asthma and COPD Program at Northwestern University Feinberg School of Medicine and Northwestern Memorial Hospital.
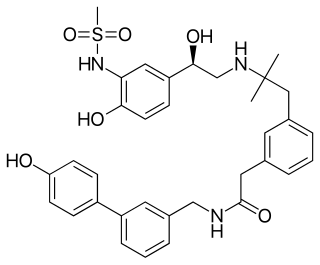
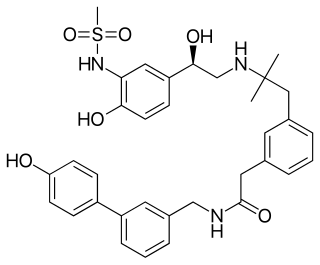
PF-610355 is an inhalable ultra-long-acting β2 adrenoreceptor agonist (ultra-LABA) that was investigated as a treatment of asthma and COPD by Pfizer. It utilizes a sulfonamide agonist headgroup, that confers high levels of intrinsic crystallinity that could relate to the acidic sulfonamide motif supporting a zwitterionic form in the solid state. Optimization of pharmacokinetic properties minimized systemic exposure following inhalation and reduced systemically-mediated adverse events. Its in vivo duration on action confirmed its potential for once-daily use in humans.
Airway basal cells are found deep in the respiratory epithelium, attached to, and lining the basement membrane.
Donna Elizabeth Davies is a British biochemist and professor of respiratory cell and molecular biology at the University of Southampton. In 2003, Davies was the co-founder of Synairgen, an interferon-beta drug designed to treat patients with asthma and chronic obstructive pulmonary disease.

Francesco Blasi is an Italian Medical scientist and professor. His domain of research is respiratory medicine. He has been the president of European Respiratory Society (ERS) during 2012–13. He has served as the president of Italian Respiratory Society during 2015–17. He is presently serving as one of the board of directors of University of Milan and is the professor of respiratory medicine in department pathophysiology and transplantation in University of Milan.