Related Research Articles

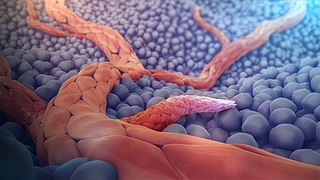
A capillary is a small blood vessel, from 5 to 10 micrometres in diameter, and is part of the microcirculation system. Capillaries are microvessels and the smallest blood vessels in the body. They are composed of only the tunica intima, consisting of a thin wall of simple squamous endothelial cells. They are the site of the exchange of many substances from the surrounding interstitial fluid, and they convey blood from the smallest branches of the arteries (arterioles) to those of the veins (venules). Other substances which cross capillaries include water, oxygen, carbon dioxide, urea, glucose, uric acid, lactic acid and creatinine. Lymph capillaries connect with larger lymph vessels to drain lymphatic fluid collected in microcirculation.
Angiogenesis is the physiological process through which new blood vessels form from pre-existing vessels, formed in the earlier stage of vasculogenesis. Angiogenesis continues the growth of the vasculature mainly by processes of sprouting and splitting, but processes such as coalescent angiogenesis, vessel elongation and vessel cooption also play a role. Vasculogenesis is the embryonic formation of endothelial cells from mesoderm cell precursors, and from neovascularization, although discussions are not always precise. The first vessels in the developing embryo form through vasculogenesis, after which angiogenesis is responsible for most, if not all, blood vessel growth during development and in disease.

Cell adhesion is the process by which cells interact and attach to neighbouring cells through specialised molecules of the cell surface. This process can occur either through direct contact between cell surfaces such as cell junctions or indirect interaction, where cells attach to surrounding extracellular matrix, a gel-like structure containing molecules released by cells into spaces between them. Cells adhesion occurs from the interactions between cell-adhesion molecules (CAMs), transmembrane proteins located on the cell surface. Cell adhesion links cells in different ways and can be involved in signal transduction for cells to detect and respond to changes in the surroundings. Other cellular processes regulated by cell adhesion include cell migration and tissue development in multicellular organisms. Alterations in cell adhesion can disrupt important cellular processes and lead to a variety of diseases, including cancer and arthritis. Cell adhesion is also essential for infectious organisms, such as bacteria or viruses, to cause diseases.

The endothelium is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the vessel wall. Endothelial cells form the barrier between vessels and tissue and control the flow of substances and fluid into and out of a tissue.

Pericytes are multi-functional mural cells of the microcirculation that wrap around the endothelial cells that line the capillaries throughout the body. Pericytes are embedded in the basement membrane of blood capillaries, where they communicate with endothelial cells by means of both direct physical contact and paracrine signaling. The morphology, distribution, density and molecular fingerprints of pericytes vary between organs and vascular beds. Pericytes help to maintain homeostatic and hemostatic functions in the brain, one of the organs with higher pericyte coverage, and also sustain the blood–brain barrier. These cells are also a key component of the neurovascular unit, which includes endothelial cells, astrocytes, and neurons. Pericytes have been postulated to regulate capillary blood flow and the clearance and phagocytosis of cellular debris in vitro. Pericytes stabilize and monitor the maturation of endothelial cells by means of direct communication between the cell membrane as well as through paracrine signaling. A deficiency of pericytes in the central nervous system can cause increased permeability of the blood–brain barrier.

Kinase insert domain receptor also known as vascular endothelial growth factor receptor 2 (VEGFR-2) is a VEGF receptor. KDR is the human gene encoding it. KDR has also been designated as CD309. KDR is also known as Flk1.

Cadherin-2 also known as Neural cadherin (N-cadherin), is a protein that in humans is encoded by the CDH2 gene. CDH2 has also been designated as CD325 . Cadherin-2 is a transmembrane protein expressed in multiple tissues and functions to mediate cell–cell adhesion. In cardiac muscle, Cadherin-2 is an integral component in adherens junctions residing at intercalated discs, which function to mechanically and electrically couple adjacent cardiomyocytes. Alterations in expression and integrity of Cadherin-2 has been observed in various forms of disease, including human dilated cardiomyopathy. Variants in CDH2 have also been identified to cause a syndromic neurodevelopmental disorder.

Cadherin-5, or VE-cadherin, also known as CD144, is a type of cadherin. It is encoded by the human gene CDH5.
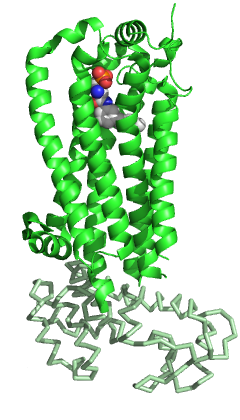
Sphingosine-1-phosphate receptor 1, also known as endothelial differentiation gene 1 (EDG1) is a protein that in humans is encoded by the S1PR1 gene. S1PR1 is a G-protein-coupled receptor which binds the bioactive signaling molecule sphingosine 1-phosphate (S1P). S1PR1 belongs to a sphingosine-1-phosphate receptor subfamily comprising five members (S1PR1-5). S1PR1 was originally identified as an abundant transcript in endothelial cells and it has an important role in regulating endothelial cell cytoskeletal structure, migration, capillary-like network formation and vascular maturation. In addition, S1PR1 signaling is important in the regulation of lymphocyte maturation, migration and trafficking.

Angiogenic factor with G patch and FHA domains 1 is a protein that in humans is encoded by the AGGF1 gene.

Napoleone Ferrara is an Italian-American molecular biologist who joined University of California, San Diego Moores Cancer Center in 2013 after a career in Northern California at the biotechnology giant Genentech, where he pioneered the development of new treatments for angiogenic diseases such as cancer, age-related macular degeneration (AMD), and diabetic retinopathy. At Genentech, he discovered VEGF—and made the first anti-VEGF antibody—which suppresses growth of a variety of tumors. These findings helped lead to development of the first clinically available angiogenesis inhibitor, bevacizumab (Avastin), which prevents the growth of new blood vessels into a solid tumor and which has become part of standard treatment for a variety of cancers. Ferrara's work led also to the development of ranibizumab (Lucentis), a drug that is highly effective at preventing vision loss in intraocular neovascular disorders.

Vasculogenic mimicry (VM) is a strategy used by tumors to ensure sufficient blood supply is brought to its cells through establishing new tumor vascularization. This process is similar to tumor angiogenesis; on the other hand vascular mimicry is unique in that this process occurs independent of endothelial cells. Vasculature is instead developed de novo by cancer cells, which under stress conditions such as hypoxia, express similar properties to stem cells, capable of differentiating to mimic the function of endothelial cells and form vasculature-like structures. The ability of tumors to develop and harness nearby vasculature is considered one of the hallmarks of cancer disease development and is thought to be closely linked to tumor invasion and metastasis. Vascular mimicry has been observed predominantly in aggressive and metastatic cancers and has been associated with negative tumor characteristics such as increased metastasis, increased tissue invasion, and overall poor outcomes for patient survival. Vascular mimicry poses a serious problem for current therapeutic strategies due to its ability to function in the presence of Anti-angiogenic therapeutic agents. In fact, such therapeutics have been found to actually drive VM formation in tumors, causing more aggressive and difficult to treat tumors to develop.

Vsevolod Tkachuk is a Soviet and Russian biochemist. Academician of RAMS and RAS. Dean of the Faculty of fundamental medicine of Lomonosov Moscow State University. Director of institute of regenerative medicine in Lomonosov Moscow State University and president of National regenerative medicine society.

Tumor-associated endothelial cells or tumor endothelial cells (TECs) refers to cells lining the tumor-associated blood vessels that control the passage of nutrients into surrounding tumor tissue. Across different cancer types, tumor-associated blood vessels have been discovered to differ significantly from normal blood vessels in morphology, gene expression, and functionality in ways that promote cancer progression. There has been notable interest in developing cancer therapeutics that capitalize on these abnormalities of the tumor-associated endothelium to destroy tumors.

Kairbaan Hodivala-Dilke, FMedSci is an English cell biologist who has made significant contributions to the understanding of the cellular and molecular biology of the tumour microenvironment and in particular angiogenesis. She is Professor of Angiogenesis and the Tumour Microenvironment and Deputy Institute Director of Barts Cancer Institute, Queen Mary University of London. In 2015 she was awarded the Hooke medal from the British Society for Cell Biology and EMBO membership.
Eli Keshet is an Israeli biochemist and professor of molecular biology at the Hebrew University of Jerusalem. He is the laureate of the 2021 Israel Prize for Life Sciences.
Élisabeth Tournier-Lasserve is a French neurologist, medical geneticist, university professor and hospital practitioner in genetics. Together with three colleagues, she was the co-recipient of the Brain Prize in 2019, the world's largest brain research prize.
Esther Lutgens is a Dutch physician and molecular biologist who is Professor of Vascular Immunopathology at Amsterdam University Medical Centre. She studies the modulation of co-stimulatory pathways and the immune system.
Anjali Kusumbe is a British-Indian biologist who is the Head of the Tissue and Tumour Microenvironments Group at the Medical Research Council Weatherall Institute of Molecular Medicine at the University of Oxford. She was awarded the Royal Microscopical Society Award for Life Sciences in 2022.
Katie Bentley is a British computer scientist who is group leader in the Cellular Adaptive Behaviour Laboratory at the Francis Crick Institute and an academic at King's College London. Her research considers computational simulations of cellular interactions.
References
- 1 2 3 4 5 "CV: Elisabetta Dejana" (PDF). Onda, Osservatorio Nazionale sulla Salute della Donna. Retrieved 12 May 2021.
- 1 2 3 4 "Elisabetta Dejana". IFOM. Retrieved 12 May 2021.
- 1 2 3 4 5 "2016 Navbo Earl P. Benditt Award - Elisabetta Dejana, University of Uppsala". NAVBO. Retrieved 12 May 2021.
- ↑ "Elisabetta Dejana – New strategies to inhibit tumour angiogenesis". Uppsala University. Retrieved 12 May 2021.
- 1 2 "Elisabetta Dejana, Prix International 2018". Inserm. Retrieved 12 May 2021.
- ↑ "Outstanding Contribution to Science Medal". The William Harvey Research Institute. Archived from the original on 12 May 2021. Retrieved 12 May 2021.
- ↑ "PREMI "ANTONIO FELTRINELLI" 2014" (PDF). Accademia dei Lincei. Retrieved 12 May 2021.
- ↑ "Fondation Lefoulon-Delalande". Institute de France Grands Prix des Fondations. Retrieved 12 May 2021.