Related Research Articles

Over-the-counter (OTC) drugs are medicines sold directly to a consumer without a requirement for a prescription from a healthcare professional, as opposed to prescription drugs, which may be supplied only to consumers possessing a valid prescription. In many countries, OTC drugs are selected by a regulatory agency to ensure that they contain ingredients that are safe and effective when used without a physician's care. OTC drugs are usually regulated according to their active pharmaceutical ingredient (API) rather than final products. By regulating APIs instead of specific drug formulations, governments allow manufacturers the freedom to formulate ingredients, or combinations of ingredients, into proprietary mixtures.

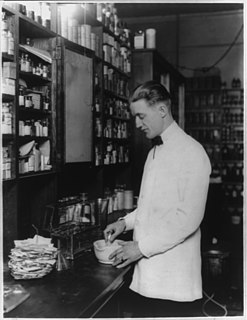
A pharmacist, also known as a chemist or a druggist, is a health professional who specializes in the preparation, properties, effects, interactions and use of medicines. The pharmacist provides pharmaceutical care to patients, as well as basic primary health care services. Using knowledge of the mechanism of action of drugs, the pharmacist understands how they should be used to achieve maximum benefit, minimal side effects and to avoid drug interactions. Pharmacists undergo university or graduate-level education to understand the biochemical mechanisms and actions of drugs, drug uses, therapeutic roles, side effects, potential drug interactions, and monitoring parameters. This is mated to anatomy, physiology, and pathophysiology. Pharmacists interpret and communicate this specialized knowledge to patients, physicians, and other health care providers.

Pharmacy is the clinical health science that links medical science with chemistry and it is charged with the discovery, production, disposal, safe and effective use, and control of medications and drugs. The practice of pharmacy requires excellent knowledge of drugs, their mechanism of action, side effects, interactions, mobility and toxicity. At the same time, it requires knowledge of treatment and understanding of the pathological process. Some specialties of pharmacists, such as that of clinical pharmacists, require other skills, e.g. knowledge about the acquisition and evaluation of physical and laboratory data.

A prescription, often abbreviated ℞ or Rx, is a formal communication from a physician or other registered health-care professional to a pharmacist, authorizing them to dispense a specific prescription drug for a specific patient. Historically, it was a physician's instruction to an apothecary listing the materials to be compounded into a treatment—the symbol ℞ comes from the first word of a medieval prescription, Latin: Recipere, that gave the list of the materials to be compounded.

A pharmacy technician is a title-protected, licensed health care provider who performs pharmacy-related functions, working collaboratively with a licensed pharmacist.
In the field of pharmacy, compounding is preparation of a custom formulation of a medication to fit a unique need of a patient that cannot be met with commercially available products. This may be done for medical reasons, such as administration in a different format, to avoid a non-active ingredient the patient is allergic to, or to provide an exact dose that isn't commercially available. Medically necessary compounding is referred to as "traditional" compounding. It may also be done for medically optional reasons, such as preference of flavor or texture, or dietary restrictions.
Pharmaceutical policy is a branch of health policy that deals with the development, provision and use of medications within a health care system. It embraces drugs, biologics, vaccines and natural health products.

Clinical pharmacy is the branch of pharmacy in which clinical pharmacists provide direct patient care that optimizes the use of medication and promotes health, wellness, and disease prevention. Clinical pharmacists care for patients in all health care settings but the clinical pharmacy movement initially began inside hospitals and clinics. Clinical pharmacists often work in collaboration with physicians, physician assistants, nurse practitioners, and other healthcare professionals. Clinical pharmacists can enter into a formal collaborative practice agreement with another healthcare provider, generally one or more physicians, that allows pharmacists to prescribe medications and order laboratory tests.
Pharmacy residency is education a pharmacist can pursue beyond the degree required for licensing as a pharmacist. A pharmacy residency program allows for the implementation of skill set and knowledge acquired in pharmacy school through interaction with the public either in a hospital setting or community practice. The program is done over a span of about 2yrs after graduation from pharmacy school and licensure as a pharmacist and helps improve the resume of a pharmacist so as to increase chances of obtaining employment outside community practice.

A pharmacy is a retail shop which provides pharmaceutical drugs, among other products. At the pharmacy, a pharmacist oversees the fulfillment of medical prescriptions and is available to counsel patients about prescription and over-the-counter drugs or about healthcare and wellness issues. A typical pharmacy would be in the commercial area of a community. Mail-order dispensing is a recent development.
Electronic prescription is the computer-based electronic generation, transmission, and filling of a medical prescription, taking the place of paper and faxed prescriptions. E-prescribing allows a physician, physician assistant, pharmacist, or nurse practitioner to use digital prescription software to electronically transmit a new prescription or renewal authorization to a community or mail-order pharmacy. It outlines the ability to send error-free, accurate, and understandable prescriptions electronically from the healthcare provider to the pharmacy. E-prescribing is meant to reduce the risks associated with traditional prescription script writing. It is also one of the major reasons for the push for electronic medical records. By sharing medical prescription information, e-prescribing seeks to connect the patient's team of healthcare providers to facilitate knowledgeable decision making.
Pharmacy automation involves the mechanical processes of handling and distributing medications. Any pharmacy task may be involved, including counting small objects ; measuring and mixing powders and liquids for compounding; tracking and updating customer information in databases ; and inventory management. This article focuses on the changes that have taken place in the local, or community pharmacy since the 1960s.
The Ohio Automated Rx Reporting System (OARRS) is Ohio's state Prescription Monitoring Program (PMP) and is controlled by the Ohio State Board of Pharmacy. The law permitting the Board of Pharmacy to create the PMP was signed on March 18, 2005, and became effective January 1, 2006. The OARRS program began operation on October 2, 2006. The law is available to read in the Drug Laws of Ohio pages C-50 through C-54. The Ohio State Board of Pharmacy is responsible for collecting and verifying data for prescriptions that the Drug Enforcement Administration (DEA) classifies Schedule II-V as well as carisoprodol and tramadol prescriptions.
Fred Henry Mills, Jr., is an American pharmacist, banker, and politician from Parks, Louisiana currently serving as a Republican member of the Louisiana State Senate, having won a special election on January 22, 2011. Mills had previously represented District 46 in the Louisiana House of Representatives.
Practicing without a license is the act of working without the licensure offered for that occupation, in a particular jurisdiction. Most activities that require licensure also have penalties for practicing without a valid, current license. In some jurisdictions, a license is offered but not required for some professions.

Telepharmacy is the delivery of pharmaceutical care via telecommunications to patients in locations where they may not have direct contact with a pharmacist. It is an instance of the wider phenomenon of telemedicine, as implemented in the field of pharmacy. Telepharmacy services include drug therapy monitoring, patient counseling, prior authorization and refill authorization for prescription drugs, and monitoring of formulary compliance with the aid of teleconferencing or videoconferencing. Remote dispensing of medications by automated packaging and labeling systems can also be thought of as an instance of telepharmacy. Telepharmacy services can be delivered at retail pharmacy sites or through hospitals, nursing homes, or other medical care facilities.

R v Lee is the leading case in England and Wales concerning erroneous professional dispensing of a controlled medicine. The case was considered by foremost judges with a conviction in the Central Criminal Court of England and Wales in front of its President, the Recorder of London, and its partly successful appeal in the binding precedent-level Court of Appeal. The case confirmed that a serious error in giving a vulnerable customer a potent drug that does not match in any way the prescription, where such action is not the primary causation of any death or suffering, can result in a prosecution of the responsible pharmacist, with up to 2 years imprisonment, depending on the circumstances.
A collaborative practice agreement (CPA) is a legal document in the United States that establishes a legal relationship between clinical pharmacists and collaborating physicians that allows for pharmacists to participate in collaborative drug therapy management (CDTM).
Surfing the Healthcare Tsunami: Bring Your Best Board is a made for television documentary that explores medical errors and waste in healthcare. It was broadcast globally on the Discovery Channel in 2012. It references federally-funded studies in the United States and news footage to support the claim that healthcare workers are afraid to speak up when medical errors occur in hospitals. The documentary covers solutions to preventable system failures causing harm. It aired four times on the Discovery Channel commercial-free in North America, Germany, the U.K., France, and other Western European countries including Sweden. It premiered at the National Press Club on April 27, 2012 after a short speech by Captain Sully Sullenberger who was featured in the film. The film was screened at the Texas Health Care Quality Improvement Awards on May 3, 2012.
Autonomous pharmacy is an approach to medication management that seeks to create a more automated and data-driven process for medication inventory and dispensing. The main concept behind autonomous pharmacy is to use technology in place of manual medication processes in order to help healthcare providers reduce medication errors, decrease costs and save staff time. Autonomous pharmacy may use a combination of hardware, software and technology-enabled services to allow pharmacists to more effectively manage medication dispersal.
References
- ↑ John Kuntz (13 May 2009). "Ex-pharmacist Eric Cropp found guilty in medication death of Emily Jerry, 2". The Plain Dealer. Retrieved 2016-05-29.
- ↑ "Emily's Law Revisited: The Pharmacist, the Family, and the Medication Error That Changed Their Lives" (PDF). Archived from the original (PDF) on 2014-02-20. Retrieved 2014-02-03.
- ↑ Jesse C. Vivian (November 19, 2009). "Criminalization of Medication Errors". U.S. Pharmacist.
- ↑ "Emily's Law Signed by Governor". National Pharmacy Technician Association. 2009-01-07. Archived from the original on 2014-02-03. Retrieved 2016-05-29.
- ↑ "Laws, Acts, and Legislation" . Retrieved 2016-05-29.
- ↑ "Archived copy". Archived from the original on 2014-02-22. Retrieved 2014-02-03.
{{cite web}}: CS1 maint: archived copy as title (link)