Related Research Articles

Aspirin, also known as acetylsalicylic acid (ASA), is a nonsteroidal anti-inflammatory drug (NSAID) used to reduce pain, fever, and/or inflammation, and as an antithrombotic. Specific inflammatory conditions which aspirin is used to treat include Kawasaki disease, pericarditis, and rheumatic fever.

Migraine is a genetically-influenced complex neurological disorder characterized by episodes of moderate-to-severe headache, most often unilateral and generally associated with nausea and light and sound sensitivity. Other characterizing symptoms may include nausea, vomiting, cognitive dysfunction, allodynia, and dizziness. Exacerbation of headache symptoms during physical activity is another distinguishing feature.
Non-steroidal anti-inflammatory drugs (NSAID) are members of a therapeutic drug class which reduces pain, decreases inflammation, decreases fever, and prevents blood clots. Side effects depend on the specific drug, its dose and duration of use, but largely include an increased risk of gastrointestinal ulcers and bleeds, heart attack, and kidney disease.

A placebo is a substance or treatment which is designed to have no therapeutic value. Common placebos include inert tablets, inert injections, sham surgery, and other procedures.

Diclofenac, sold under the brand name Voltaren, among others, is a nonsteroidal anti-inflammatory drug (NSAID) used to treat pain and inflammatory diseases such as gout. It can be taken orally, inserted rectally as a suppository, injected intramuscularly (IM), injected intravenously (IV), or applied to the skin topically. Improvements in pain last up to eight hours. It is also available in combination with misoprostol in an effort to decrease stomach problems.
Cyclooxygenase-2 inhibitors, also known as coxibs, are a type of nonsteroidal anti-inflammatory drug (NSAID) that directly target cyclooxygenase-2 (COX-2), an enzyme responsible for inflammation and pain. Targeting selectivity for COX-2 reduces the risk of peptic ulceration and is the main feature of celecoxib, rofecoxib, and other members of this drug class.
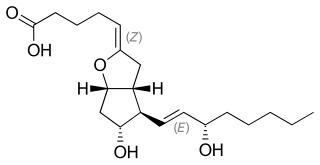
Prostacyclin (also called prostaglandin I2 or PGI2) is a prostaglandin member of the eicosanoid family of lipid molecules. It inhibits platelet activation and is also an effective vasodilator.
A nocebo effect is said to occur when a patient's negative expectations for a treatment cause the treatment to have a worse effect than it otherwise would have. For example, when a patient anticipates a side effect of a medication, they can experience that effect even if the "medication" is actually an inert substance. The complementary concept, the placebo effect, is said to occur when positive expectations improve an outcome. The nocebo effect is also said to occur in someone who falls ill owing to the erroneous belief that they were exposed to a physical phenomenon they believe is harmful, such as EM radiation.

Hyperalgesia is an abnormally increased sensitivity to pain, which may be caused by damage to nociceptors or peripheral nerves and can cause hypersensitivity to stimulus. Prostaglandins E and F are largely responsible for sensitizing the nociceptors. Temporary increased sensitivity to pain also occurs as part of sickness behavior, the evolved response to infection.

Indometacin, also known as indomethacin, is a nonsteroidal anti-inflammatory drug (NSAID) commonly used as a prescription medication to reduce fever, pain, stiffness, and swelling from inflammation. It works by inhibiting the production of prostaglandins, endogenous signaling molecules known to cause these symptoms. It does this by inhibiting cyclooxygenase, an enzyme that catalyzes the production of prostaglandins.
A prostaglandin antagonist is a hormone antagonist acting upon one or more prostaglandins, a subclass of eicosanoid compounds which function as signaling molecules in numerous types of animal tissues.
Pain tolerance is the maximum level of pain that a person is able to tolerate. Pain tolerance is distinct from pain threshold. The perception of pain that goes in to pain tolerance has two major components. First is the biological component—the headache or skin prickling that activates pain receptors. Second is the brain’s perception of pain—how much focus is spent paying attention to or ignoring the pain. The brain’s perception of pain is a response to signals from pain receptors that sensed the pain in the first place.

Proglumide (Milid) is a drug that inhibits gastrointestinal motility and reduces gastric secretions. It acts as a cholecystokinin antagonist, which blocks both the CCKA and CCKB subtypes. It was used mainly in the treatment of stomach ulcers, although it has now been largely replaced by newer drugs for this application.

Aspirin causes several different effects in the body, mainly the reduction of inflammation, analgesia, the prevention of clotting, and the reduction of fever. Much of this is believed to be due to decreased production of prostaglandins and TXA2. Aspirin's ability to suppress the production of prostaglandins and thromboxanes is due to its irreversible inactivation of the cyclooxygenase (COX) enzyme. Cyclooxygenase is required for prostaglandin and thromboxane synthesis. Aspirin acts as an acetylating agent where an acetyl group is covalently attached to a serine residue in the active site of the COX enzyme. This makes aspirin different from other NSAIDs, which are reversible inhibitors; aspirin creates an allosteric change in the structure of the COX enzyme. However, other effects of aspirin, such as uncoupling oxidative phosphorylation in mitochondria, and the modulation of signaling through NF-κB, are also being investigated. Some of its effects are like those of salicylic acid, which is not an acetylating agent.
The word placebo was used in a medicinal context in the late 18th century to describe a "commonplace method or medicine" and in 1811 it was defined as "any medicine adapted more to please than to benefit the patient". Although this definition contained a derogatory implication, it did not necessarily imply that the remedy had no effect.

Emoxypine (2-ethyl-6-methyl-3-hydroxypyridine), also known as Mexidol or Mexifin, a succinate salt, is chemical compound which is claimed by its manufacturer, the Russian company Pharmasoft Pharmaceuticals, to have antioxidant and actoprotector properties,, but these purported properties of emoxypine have not been proven. Its chemical structure resembles that of pyridoxine (a type of vitamin B6).
Tor D. Wager is the Diana L. Taylor Distinguished Professor in Neuroscience at Dartmouth College, as well as the director of the Cognitive and Affective Neuroscience Laboratory at this university. He is known for his research into the placebo effect and into the way the brain processes pain.
Placebo analgesia occurs when the administration of placebos leads to pain relief. Because placebos by definition lack active ingredients, the effect of placebo analgesia is considered to result from the patient's belief that they are receiving an analgesic drug or other medical intervention. It has been shown that, in some cases, the endogenous opioid system is critical for mediating placebo analgesia, as evidenced by the ability of such analgesia to be reduced by the opioid antagonist naloxone. However, it is also possible for placebo analgesia to be mediated by non-opioid mechanisms, in which case it would not be affected by naloxone. Other research has indicated that the human spinal cord, prefrontal cortex, and rostral anterior cingulate cortex also play a role in placebo analgesia.
Prostaglandin inhibitors are drugs that inhibit the synthesis of prostaglandin in human body. There are various types of prostaglandins responsible for different physiological reactions such as maintaining the blood flow in stomach and kidney, regulating the contraction of involuntary muscles and blood vessels, and act as a mediator of inflammation and pain. Cyclooxygenase (COX) and Phospholipase A2 are the major enzymes involved in prostaglandin production, and they are the drug targets for prostaglandin inhibitors. There are mainly 2 classes of prostaglandin inhibitors, namely non- steroidal anti- inflammatory drugs (NSAIDs) and glucocorticoids. In the following sections, the medical uses, side effects, contraindications, toxicity and the pharmacology of these prostaglandin inhibitors will be discussed.

Sonlicromanol (KH176) is a clinical-stage oral drug compound developed by Khondrion as a potential treatment for inherited mitochondrial diseases, such as Leigh's Disease, MELAS and LHON. Due to dysfunctional mitochondria, an increased level of cellular reactive oxygen species (ROS) is observed in these patients, causing a wide range of symptoms. The active metabolite of Sonlicromanol has several mechanisms of action, acting both as antioxidant and as reactive oxygen species (ROS)-redox modulator. Through selective suppression of microsomal prostaglandin E synthase-1 (mPGES-1), Sonlicromanol even has potency as anti-cancer drug for mPGES-1 overexpressing cancer like prostate cancer. Currently, Sonlicromanol is in phase II clinical trial in the KHENERGYZE, KHENEREXT and KHENERGYC studies as potent candidate in treatment for mitochondrial diseases.
References
- ↑ "Placebo Effects in Psychology". Oxford Bibliographies. Retrieved 17 March 2022.
- ↑ Planès, Sara; Villier, Céline; Mallaret, Michel (17 March 2016). "The nocebo effect of drugs". Pharmacology Research & Perspectives. 4 (2): e00208. doi:10.1002/prp2.208. ISSN 2052-1707. PMC 4804316 . PMID 27069627.
- ↑ Benedetti, Fabrizio (3 March 2022). "The science of placebos is fuelling quackery". Knowable Magazine. doi: 10.1146/knowable-030222-3 . S2CID 247265071 . Retrieved 17 March 2022.
- 1 2 Silberman, Steve (24 August 2009). "Placebos Are Getting More Effective. Drugmakers Are Desperate to Know Why". Wired. Retrieved 25 October 2014.
- ↑ Neergaard, Lauren (28 November 2005). "Expecting benefit really can help healing". USA Today. Retrieved 25 October 2014.
- ↑ Benedetti, F.; Pollo, A.; Colloca, L. (31 October 2007). "Opioid-Mediated Placebo Responses Boost Pain Endurance and Physical Performance: Is It Doping in Sport Competitions?". Journal of Neuroscience. 27 (44): 11934–11939. doi: 10.1523/JNEUROSCI.3330-07.2007 . PMC 6673345 . PMID 17978033.
- ↑ "How to cheat without cheating". The Economist. 1 November 2007. Retrieved 3 August 2015.
- ↑ Benedetti, Fabrizio; Carlino, Elisa; Pollo, Antonella (30 June 2010). "How Placebos Change the Patient's Brain". Neuropsychopharmacology. 36 (1): 339–354. doi:10.1038/npp.2010.81. PMC 3055515 . PMID 20592717.
- ↑ Benedetti, F.; Amanzio, M.; Vighetti, S.; Asteggiano, G. (15 November 2006). "The Biochemical and Neuroendocrine Bases of the Hyperalgesic Nocebo Effect". Journal of Neuroscience. 26 (46): 12014–12022. doi: 10.1523/JNEUROSCI.2947-06.2006 . PMC 6674855 . PMID 17108175.
- ↑ Sarchet, Penny (13 November 2011). "The nocebo effect: Wellcome Trust science writing prize essay". The Guardian. Retrieved 25 October 2014.
- ↑ Scudellari, Megan (1 July 2013). "Worried Sick". The Scientist. Retrieved 26 October 2014.
- ↑ Benedetti, Fabrizio; Durando, Jennifer; Vighetti, Sergio (May 2014). "Nocebo and placebo modulation of hypobaric hypoxia headache involves the cyclooxygenase-prostaglandins pathway". Pain. 155 (5): 921–928. doi:10.1016/j.pain.2014.01.016. hdl: 2318/151583 . PMID 24462931. S2CID 207310855.
- ↑ Robson, David (11 February 2015). "The contagious thought that could kill you". BBC. Retrieved 11 February 2015.
- ↑ Vance, Erik (27 July 2010). "Get to Know the Placebo Effect". Chicago Tribune. Archived from the original on July 23, 2018. Retrieved 25 October 2014.
- ↑ Brody, Howard A. (9 April 2009). "Book Review Placebo Effects: Understanding the Mechanisms in Health and Disease By Fabrizio Benedetti. 295 pp., illustrated. New York, Oxford University Press, 2009. $59.95. 978-0-19-955912-1". New England Journal of Medicine. 360 (15): 1576–1577. doi:10.1056/NEJMbkrev0810817.
- ↑ Benedetti, Fabrizio (May 2011). "Ask the Experts: Is there a place for placebo analgesia in everyday clinical practice?". Pain Management. 1 (3): 211–212. doi:10.2217/pmt.11.16. ISSN 1758-1869. PMID 24646386.