Related Research Articles
Hemiparesis, or unilateral paresis, is weakness of one entire side of the body. Hemiplegia is, in its most severe form, complete paralysis of half of the body. Hemiparesis and hemiplegia can be caused by different medical conditions, including congenital causes, trauma, tumors, or stroke.
Spasticity is a feature of altered skeletal muscle performance with a combination of paralysis, increased tendon reflex activity, and hypertonia. It is also colloquially referred to as an unusual "tightness", stiffness, or "pull" of muscles.
Activities of daily living is a term used in healthcare to refer to people's daily self-care activities. The concept of ADLs was originally proposed in the 1950s by Sidney Katz and his team at the Benjamin Rose Hospital in Cleveland, Ohio and has been added to and refined by a variety of researchers since that time. Health professionals often use a person's ability or inability to perform ADLs as a measurement of their functional status, particularly in regard to people post injury, with disabilities and the elderly. Younger children often require help from adults to perform ADLs, as they have not yet developed the skills necessary to perform them independently.

Neurotrauma, brain damage or brain injury (BI) is the destruction or degeneration of brain cells. Brain injuries occur due to a wide range of internal and external factors. In general, brain damage refers to significant, undiscriminating trauma-induced damage, while neurotoxicity typically refers to selective, chemically induced neuron damage.
Rehabilitation of sensory and cognitive function typically involves methods for retraining neural pathways or training new neural pathways to regain or improve neurocognitive functioning that have been diminished by disease or trauma. Three common neuropsychological problems treatable with rehabilitation are attention deficit/hyperactivity disorder (ADHD), concussion, and spinal cord injury. Rehabilitation research and practices are a fertile area for clinical neuropsychologists, rehabilitation psychologists, and others.

A spinal cord injury (SCI) is damage to the spinal cord that causes temporary or permanent changes in its function. Symptoms may include loss of muscle function, sensation, or autonomic function in the parts of the body served by the spinal cord below the level of the injury. Injury can occur at any level of the spinal cord and can be complete, with a total loss of sensation and muscle function at lower sacral segments, or incomplete, meaning some nervous signals are able to travel past the injured area of the cord up to the Sacral S4-5 spinal cord segments. Depending on the location and severity of damage, the symptoms vary, from numbness to paralysis, including bowel or bladder incontinence. Long term outcomes also range widely, from full recovery to permanent tetraplegia or paraplegia. Complications can include muscle atrophy, loss of voluntary motor control, spasticity, pressure sores, infections, and breathing problems.
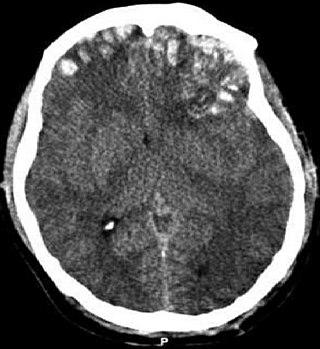
A traumatic brain injury (TBI), also known as an intracranial injury, is an injury to the brain caused by an external force. TBI can be classified based on severity, mechanism, or other features. Head injury is a broader category that may involve damage to other structures such as the scalp and skull. TBI can result in physical, cognitive, social, emotional and behavioral symptoms, and outcomes can range from complete recovery to permanent disability or death.

Physical medicine and rehabilitation, also known as physiatry, is a branch of medicine that aims to enhance and restore functional ability and quality of life to people with physical impairments or disabilities. This can include conditions such as spinal cord injuries, brain injuries, strokes, as well as pain or disability due to muscle, ligament or nerve damage. A physician having completed training in this field may be referred to as a physiatrist.

Central cord syndrome (CCS) is the most common form of cervical spinal cord injury. It is characterized by loss of motion and sensation in arms and hands. It usually results from trauma which causes damage to the neck, leading to major injury to the central corticospinal tract of the spinal cord. The syndrome is more common in people over the age of 50 because osteoarthritis in the neck region causes weakening of the vertebrae. CCS most frequently occurs among older persons with cervical spondylosis, however, it also may occur in younger individuals.
Neurorehabilitation is a complex medical process which aims to aid recovery from a nervous system injury, and to minimize and/or compensate for any functional alterations resulting from it.
Shepherd Center is a private, not-for profit hospital in Atlanta, Georgia. Founded in 1975, the 152-bed hospital focuses on the medical treatment, research and rehabilitation for people with spinal cord injury and disease, acquired brain injury, multiple sclerosis, chronic pain and other neuromuscular problems.
Post-traumatic amnesia (PTA) is a state of confusion that occurs immediately following a traumatic brain injury (TBI) in which the injured person is disoriented and unable to remember events that occur after the injury. The person may be unable to state their name, where they are, and what time it is. When continuous memory returns, PTA is considered to have resolved. While PTA lasts, new events cannot be stored in the memory. About a third of patients with mild head injury are reported to have "islands of memory", in which the patient can recall only some events. During PTA, the patient's consciousness is "clouded". Because PTA involves confusion in addition to the memory loss typical of amnesia, the term "post-traumatic confusional state" has been proposed as an alternative.
MedStar National Rehabilitation Network is located in Washington, D.C., and specializes in treating persons with physical disabilities, including spinal cord injury, brain injury, stroke, arthritis, amputation, multiple sclerosis, post-polio syndrome, orthopedic, and other neurological conditions. National Rehabilitation Hospital was founded in 1986 by Edward A. Eckenhoff, and is a member of the MedStar Health system, the Washington, D.C.-Baltimore region's largest non-profit healthcare organization.
Magee Rehabilitation Hospital, part of Jefferson Health, founded in 1958, is a 96-bed specialty medical rehabilitation hospital providing physical and cognitive rehabilitation services. Magee's flagship facility is located in Center City Philadelphia. In addition to the main campus that offers comprehensive services for spinal cord injury, brain injury, stroke, orthopaedic replacement, amputation, pain management and work injury, Magee provides an expanding outpatient network serving the surrounding communities. In 1985, Magee's brain injury rehabilitation program became the first in the nation to be accredited by the Commission on the Accreditation of Rehabilitation Facilities. Magee partnered with Jefferson Hospital to create one of the nation's 14 federally designated centers for spinal cord injury rehabilitation. Magee has been rated one of America's leading rehabilitation hospitals by U.S. News & World Report. Magee provides treatment to more than 5,000 individuals annually. Magee is authorized to treat wounded military personnel returning from war. Magee is not an Obligated Group Affiliate.

Bethesda Hospital is currently a Covid-19 only hospital located in St. Paul, Minnesota, United States. It is accredited by the Joint Commission and the Commission on Accreditation of Rehabilitation Facilities (CARF). It previously was a member of the HealthEast Care System.

Cognitive rehabilitation refers to a wide range of evidence-based interventions designed to improve cognitive functioning in brain-injured or otherwise cognitively impaired individuals to restore normal functioning, or to compensate for cognitive deficits. It entails an individualized program of specific skills training and practice plus metacognitive strategies. Metacognitive strategies include helping the patient increase self-awareness regarding problem-solving skills by learning how to monitor the effectiveness of these skills and self-correct when necessary.
When treating a person with a spinal cord injury, repairing the damage created by injury is the ultimate goal. By using a variety of treatments, greater improvements are achieved, and, therefore, treatment should not be limited to one method. Furthermore, increasing activity will increase his/her chances of recovery.
The Disability Rating Scale (DRS) was developed as a way to track a traumatic brain injury (TBI) patient from ‘Coma to Community’. The scale was used to rate the effects of injury and decide how long recovery might take. The rating gives insight into the cognitive impairment of the individual who suffered from the TBI.

Outcome measures in rehabilitation medicine are tools used to evaluate the level of disability. They can be beneficial for physicians to judge the path of patient's recovery, for researchers to compare different management protocols and for politicians in order to find the cost-effectiveness of their decisions.
Rehabilitation Psychology is a specialty area of psychology aimed at maximizing the independence, functional status, health, and social participation of individuals with disabilities and chronic health conditions overall and specifically with gaining and advancing with employment. Assessment and treatment may include the following areas: psychosocial, cognitive, behavioral, and functional status, self-esteem, coping skills, and quality of life. As the conditions experienced by patients vary widely, rehabilitation psychologists offer individualized treatment approaches. The discipline takes a holistic approach, considering individuals within their broader social context and assessing environmental and demographic factors that may enhance or impede progress.
References
- 1 2 3 4 Chumney, Douglas; Nollinger, Kristen; Shesko, Kristina; Skop, Karen; Spencer, Madeleine; Newton, Roberta A. (2010). "Ability of Functional Independence Measure to accurately predict functional outcome of stroke-specific population: Systematic review" (PDF). The Journal of Rehabilitation Research and Development. 47 (1): 17–30. doi: 10.1682/JRRD.2009.08.0140 . PMID 20437324.
- 1 2 3 Furlan, JC; Noonan, V; Singh, A; Fehlings, MG (August 2011). "Assessment of disability in patients with acute traumatic spinal cord injury: a systematic review of the literature". Journal of Neurotrauma. 28 (8): 1413–30. doi:10.1089/neu.2009.1148. PMC 3143412 . PMID 20367251.