Aphasia is an inability to comprehend or formulate language because of damage to specific brain regions. The major causes are stroke and head trauma. Aphasia can also be the result of brain tumors, brain infections, or neurodegenerative diseases, but the latter are far less prevalent.
Hemiparesis, or unilateral paresis, is weakness of one entire side of the body. Hemiplegia is, in its most severe form, complete paralysis of half of the body. Hemiparesis and hemiplegia can be caused by different medical conditions, including congenital causes, trauma, tumors, or stroke.

Neurotrauma, brain damage or brain injury (BI) is the destruction or degeneration of brain cells. Brain injuries occur due to a wide range of internal and external factors. In general, brain damage refers to significant, undiscriminating trauma-induced damage.
Rehabilitation of sensory and cognitive function typically involves methods for retraining neural pathways or training new neural pathways to regain or improve neurocognitive functioning that have been diminished by disease or trauma. The main objective outcome for rehabilitation is to assist in regaining physical abilities and improving performance. Three common neuropsychological problems treatable with rehabilitation are attention deficit/hyperactivity disorder (ADHD), concussion, and spinal cord injury. Rehabilitation research and practices are a fertile area for clinical neuropsychologists, rehabilitation psychologists, and others.

Occupational therapy (OT) is a global healthcare profession. It involves the use of assessment and intervention to develop, recover, or maintain the meaningful activities, or occupations, of individuals, groups, or communities. It is an independent health profession sometimes categorized as an allied health profession and consists of occupational therapists and occupational therapy assistants (OTA). OTs often work with people with mental health problems, disabilities, injuries, or impairments.

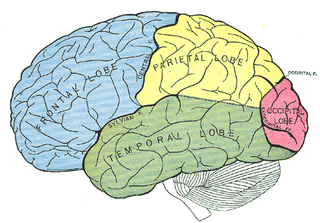
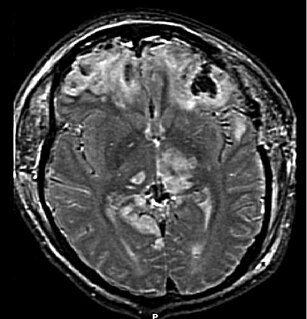
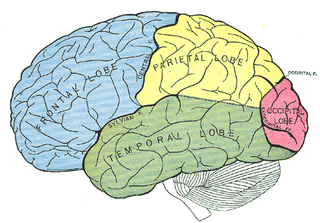
Global aphasia is a severe form of nonfluent aphasia, caused by damage to the left side of the brain, that affects receptive and expressive language skills as well as auditory and visual comprehension. Acquired impairments of communicative abilities are present across all language modalities, impacting language production, comprehension, and repetition. Patients with global aphasia may be able to verbalize a few short utterances and use non-word neologisms, but their overall production ability is limited. Their ability to repeat words, utterances, or phrases is also affected. Due to the preservation of the right hemisphere, an individual with global aphasia may still be able to express themselves through facial expressions, gestures, and intonation. This type of aphasia often results from a large lesion of the left perisylvian cortex. The lesion is caused by an occlusion of the left middle cerebral artery and is associated with damage to Broca's area, Wernicke's area, and insular regions which are associated with aspects of language.

A traumatic brain injury (TBI), also known as an intracranial injury, is an injury to the brain caused by an external force. TBI can be classified based on severity, mechanism, or other features. Head injury is a broader category that may involve damage to other structures such as the scalp and skull. TBI can result in physical, cognitive, social, emotional and behavioral symptoms, and outcomes can range from complete recovery to permanent disability or death.
Bálint's syndrome is an uncommon and incompletely understood triad of severe neuropsychological impairments: inability to perceive the visual field as a whole (simultanagnosia), difficulty in fixating the eyes, and inability to move the hand to a specific object by using vision. It was named in 1909 for the Austro-Hungarian neurologist and psychiatrist Rezső Bálint who first identified it.

Applied behavior analysis (ABA), also called behavioral engineering, is a scientific technique concerned with applying empirical approaches based upon the principles of respondent and operant conditioning to change behavior of social significance. It is the applied form of behavior analysis; the other two forms are radical behaviorism and the experimental analysis of behavior.
Behaviour therapy or behavioural psychotherapy is a broad term referring to clinical psychotherapy that uses techniques derived from behaviourism and/or cognitive psychology. It looks at specific, learned behaviours and how the environment, or other people's mental states, influences those behaviours, and consists of techniques based on learning theory, such as respondent or operant conditioning. Behaviourists who practice these techniques are either behaviour analysts or cognitive-behavioural therapists. They tend to look for treatment outcomes that are objectively measurable. Behaviour therapy does not involve one specific method, but it has a wide range of techniques that can be used to treat a person's psychological problems.
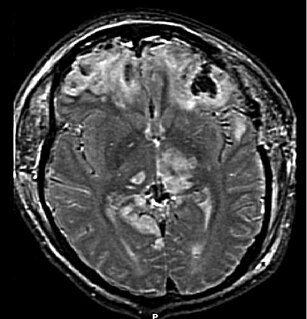
Acquired brain injury (ABI) is brain damage caused by events after birth, rather than as part of a genetic or congenital disorder such as fetal alcohol syndrome, perinatal illness or perinatal hypoxia. ABI can result in cognitive, physical, emotional, or behavioural impairments that lead to permanent or temporary changes in functioning. These impairments result from either traumatic brain injury or nontraumatic injury derived from either an internal or external source. ABI does not include damage to the brain resulting from neurodegenerative disorders.
Occupational rehabilitation is the science and practices of returning injured workers to a level of daily work activities that is appropriate to their functional and cognitive capacity related to their position of which may be influenced by the severity of a worker's injuries.
Dysexecutive syndrome (DES) consists of a group of symptoms, usually resulting from brain damage, that fall into cognitive, behavioural and emotional categories and tend to occur together. The term was introduced by Alan Baddeley to describe a common pattern of dysfunction in executive functions, such as planning, abstract thinking, flexibility and behavioural control. It is thought to be Baddeley's hypothesized working memory system and the central executive that are the hypothetical systems impaired in DES. The syndrome was once known as frontal lobe syndrome; however 'dysexecutive syndrome' is preferred because it emphasizes the functional pattern of deficits over the location of the syndrome in the frontal lobe, which is often not the only area affected. Classification code in ICD-10 - F07

Cognitive rehabilitation refers to a wide range of evidence-based interventions designed to improve cognitive functioning in brain-injured or otherwise cognitively impaired individuals to restore normal functioning, or to compensate for cognitive deficits. It entails an individualized program of specific skills training and practice plus metacognitive strategies. Metacognitive strategies include helping the patient increase self-awareness regarding problem-solving skills by learning how to monitor the effectiveness of these skills and self-correct when necessary.
Disorders of consciousness are medical conditions that inhibit consciousness. Some define disorders of consciousness as any change from complete self-awareness to inhibited or absent self-awareness and arousal. This category generally includes minimally conscious state and persistent vegetative state, but sometimes also includes the less severe locked-in syndrome and more severe but rare chronic coma. Differential diagnosis of these disorders is an active area of biomedical research. Finally, brain death results in an irreversible disruption of consciousness. While other conditions may cause a moderate deterioration or transient interruption of consciousness, they are not included in this category.
A psychological injury is the psychological or psychiatric consequence of a traumatic event or physical injury. Such an injury might result from events such as abusive behavior, whistleblower retaliation, bullying, kidnapping, rape, motor vehicular collision or other negligent action. It may cause impairments, disorders, and disabilities perhaps as an exacerbation of a pre-existing condition.
The Wechsler Test of Adult Reading (WTAR) is a neuropsychological assessment tool used to provide a measure of premorbid intelligence, the degree of Intellectual function prior to the onset of illness or disease.
Vision rehabilitation is a term for a medical rehabilitation to improve vision or low vision. In other words, it is the process of restoring functional ability and improving quality of life and independence in an individual who has lost visual function through illness or injury. Most visual rehabilitation services are focused on low vision, which is a visual impairment that cannot be fully corrected by regular eyeglasses, contact lenses, medication, or surgery. Low vision interferes with the ability to perform everyday activities. Visual impairment is caused by factors including brain damage, vision loss, and others. Of the vision rehabilitation techniques available, most center on neurological and physical approaches.
Sleep disorder is a common repercussion of traumatic brain injury (TBI). It occurs in 30%-70% of the patients suffering from TBI. TBI can be distinguished into two categories, primary and secondary damage. Primary damage includes injuries of white matter, focal contusion, cerebral edema and hematomas, mostly occurring at the moment of the trauma. Secondary damage involves the damage of neurotransmitter release, inflammatory responses, mitochondrial dysfunctions and gene activation, occurring minutes to days following the trauma. Patients with sleeping disorders following TBI suffer specifically from insomnia, sleep apnea, narcolepsy, periodic limb movement disorder and hypersomnia. Furthermore, circadian sleep-wake disorders can occur after TBI.

Eli Vakil is an Israeli clinical neuropsychologist. Vakil is a professor emeritus and former departmental chairman of the Department of Psychology, and the head of the Memory and Amnesia Lab at the Gonda (Goldschmied) Multidisciplinary Brain Research Center at Bar Ilan University. He is also director of the Rehabilitation Center for Veterans after Traumatic Brain-Injury (TBI) in Jaffa, Israel.