Related Research Articles

A seizure is a period of symptoms due to abnormally excessive or synchronous neuronal activity in the brain. Outward effects vary from uncontrolled shaking movements involving much of the body with loss of consciousness, to shaking movements involving only part of the body with variable levels of consciousness, to a subtle momentary loss of awareness. These episodes usually last less than two minutes and it takes some time to return to normal. Loss of bladder control may occur.
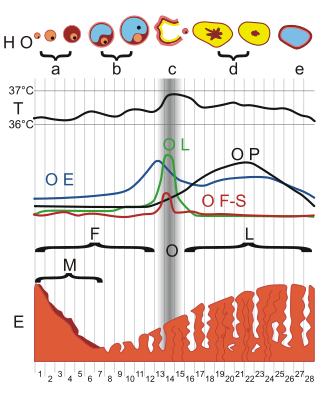
Dysmenorrhea, also known as period pain, painful periods or menstrual cramps, is pain during menstruation. Its usual onset occurs around the time that menstruation begins. Symptoms typically last less than three days. The pain is usually in the pelvis or lower abdomen. Other symptoms may include back pain, diarrhea or nausea.
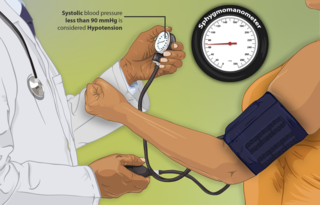
Hypotension, also known as low blood pressure, is a cardiovascular condition characterized by abnormally reduced blood pressure. Blood pressure is the force of blood pushing against the walls of the arteries as the heart pumps out blood and is indicated by two numbers, the systolic blood pressure and the diastolic blood pressure, which are the maximum and minimum blood pressures within the cardiac cycle, respectively. A systolic blood pressure of less than 90 millimeters of mercury (mmHg) or diastolic of less than 60 mmHg is generally considered to be hypotension. Different numbers apply to children. However, in practice, blood pressure is considered too low only if noticeable symptoms are present.
A headache is often present in patients with epilepsy. If the headache occurs in the vicinity of a seizure, it is defined as peri-ictal headache, which can occur either before (pre-ictal) or after (post-ictal) the seizure, to which the term ictal refers. An ictal headache itself may or may not be an epileptic manifestation. In the first case, it is defined as ictal epileptic headache or simply epileptic headache. It is a type of pain seizure that can remain isolated or be followed by other manifestations of the seizure. On the other hand, a ictal non-epileptic headache is a headache that occurs during a seizure but it is not due to an epileptic mechanism. When the headache does not occur in the vicinity of a seizure, it is defined as inter-ictal headache. In the case it's a disorder separate from epilepsy, it's a comorbidity.

Dizziness is an imprecise term that can refer to a sense of disorientation in space, vertigo, or lightheadedness. It can also refer to disequilibrium or a non-specific feeling, such as giddiness or foolishness.

Reflex syncope is a brief loss of consciousness due to a neurologically induced drop in blood pressure and/or a decrease in heart rate. Before an affected person passes out, there may be sweating, a decreased ability to see, or ringing in the ears. Occasionally, the person may twitch while unconscious. Complications of reflex syncope include injury due to a fall.
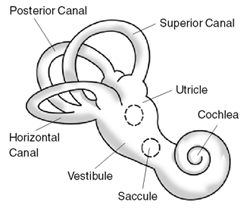
Benign paroxysmal positional vertigo (BPPV) is a disorder arising from a problem in the inner ear. Symptoms are repeated, brief periods of vertigo with movement, characterized by a spinning sensation upon changes in the position of the head. This can occur with turning in bed or changing position. Each episode of vertigo typically lasts less than one minute. Nausea is commonly associated. BPPV is one of the most common causes of vertigo.

Postural orthostatic tachycardia syndrome (POTS) is a condition characterized by an abnormally large increase in heart rate upon sitting up or standing. POTS is a disorder of the autonomic nervous system that can lead to a variety of symptoms, including lightheadedness, brain fog, blurred vision, weakness, fatigue, headaches, heart palpitations, exercise intolerance, nausea, diminished concentration, tremulousness (shaking), syncope (fainting), coldness or pain in the extremities, numbness or tingling in the extremities, chest pain, and shortness of breath. Other conditions associated with POTS include myalgic encephalomyelitis/chronic fatigue syndrome, migraine headaches, Ehlers–Danlos syndrome, asthma, autoimmune disease, vasovagal syncope, and mast cell activation syndrome. POTS symptoms may be treated with lifestyle changes such as increasing fluid, electrolyte, and salt intake, wearing compression stockings, gentle and slow postural changes, avoiding prolonged bedrest, medication, and physical therapy.

Intussusception is a medical condition in which a part of the intestine folds into the section immediately ahead of it. It typically involves the small intestine and less commonly the large intestine. Symptoms include abdominal pain which may come and go, vomiting, abdominal bloating, and bloody stool. It often results in a small bowel obstruction. Other complications may include peritonitis or bowel perforation.
Chronic paroxysmal hemicrania (CPH) is a severe debilitating unilateral headache usually affecting the area around the eye. It normally consists of multiple severe, yet short, headache attacks affecting only one side of the cranium. Retrospective surveys indicated that paroxysmal hemicrania was more common in women. However, subsequent prospective research showed an equal prevalence between females and males, with a ratio close to 1:1. Unlike in migraine, it has no neurological symptoms associated with it. CPH headaches are treated through the use of non-steroidal anti-inflammatory drugs, with indomethacin found to be especially effective in eliminating symptoms.

Fear of needles, known in medical literature as needle phobia, is the extreme fear of medical procedures involving injections or hypodermic needles.
Non-epileptic seizures (NES), also known as pseudoseizures, non-epileptic attack disorder (NEAD), functional seizures, or dissociative seizures, are paroxysmal events that appear similar to an epileptic seizure, but do not involve abnormal, rhythmic discharges of neurons in the brain. Symptoms may include shaking, loss of consciousness, and loss of bladder control.

Inappropriate sinus tachycardia (IST) is defined as sinus tachycardia that is not caused by identifiable medical ailments, a physiological reaction, or pharmaceuticals (a diagnosis of exclusion) and is accompanied by symptoms, frequently invalidating and affecting quality of life. IST symptoms include palpitations, chest discomfort, exhaustion, shortness of breath, presyncope, and syncope.
Abdominal epilepsy is a rare condition most frequently found in children, consisting of gastrointestinal disturbances caused by epileptiform seizure activity. Though a few cases of it have been reported in adults too. It has been described as a type of temporal lobe epilepsy. Responsiveness to anticonvulsants can aid in the diagnosis. Distinguishing features of abdominal epilepsy include (1) Abnormal laboratory, radiographic, and endoscopic findings revealing paroxysmal GI manifestations of unknown origin (2) CNS symptoms (3) Abnormal EEG. Most published medical literature dealing with abdominal epilepsy is in the form of individual case reports. A 2005 review article found a total of 36 cases described in the medical literature.
Alternating hemiplegia of childhood (AHC) is an ultra-rare neurological disorder named for the transient episodes, often referred to as "attacks", of hemiplegia that those with the condition experience. It typically presents before the age of 18 months. These hemiplegic attacks can cause anything from mild weakness to complete paralysis on one or both sides of the body, and they can vary greatly in duration. Attacks may also alternate from one side of the body to the other, or alternate between affecting one or both sides during a single attack. Besides hemiplegia, symptoms of the disorder include an extremely broad range of neurological and developmental impairments which are not well understood. Normally, hemiplegia and other associated symptoms cease completely with sleep, but they may recur upon waking.
Blood phobia is an extreme irrational fear of blood, a type of specific phobia. Severe cases of this fear can cause physical reactions that are uncommon in most other fears, specifically vasovagal syncope (fainting). Similar reactions can also occur with trypanophobia and traumatophobia. For this reason, these phobias are categorized as blood-injection-injury phobia by the DSM-IV. Some early texts refer to this category as "blood-injury-illness phobia."
Paroxysmal extreme pain disorder originally named familial rectal pain syndrome, is a rare disorder whose most notable features are pain in the mandibular, ocular and rectal areas as well as flushing. PEPD often first manifests at the beginning of life, perhaps even in utero, with symptoms persisting throughout life. PEPD symptoms are reminiscent of primary erythromelalgia, as both result in flushing and episodic pain, though pain is typically present in the extremities for primary erythromelalgia. Both of these disorders have recently been shown to be allelic, both caused by mutations in the voltage-gated sodium channel NaV1.7 encoded by the gene SCN9A. A different mutation in the SCN9A ion channel causes congenital insensitivity to pain.

Syncope, commonly known as fainting or passing out, is a loss of consciousness and muscle strength characterized by a fast onset, short duration, and spontaneous recovery. It is caused by a decrease in blood flow to the brain, typically from low blood pressure. There are sometimes symptoms before the loss of consciousness such as lightheadedness, sweating, pale skin, blurred vision, nausea, vomiting, or feeling warm. Syncope may also be associated with a short episode of muscle twitching. Psychiatric causes can also be determined when a patient experiences fear, anxiety, or panic; particularly before a stressful event, usually medical in nature. When consciousness and muscle strength are not completely lost, it is called presyncope. It is recommended that presyncope be treated the same as syncope.
Blood-injection-injury (BII) type phobia is a type of specific phobia characterized by the display of excessive, irrational fear in response to the sight of blood, injury, or injection, or in anticipation of an injection, injury, or exposure to blood. Blood-like stimuli may also cause a reaction. This is a common phobia with an estimated 3-4% prevalence in the general population, though it has been found to occur more often in younger and less educated groups. Prevalence of fear of needles which does not meet the BII phobia criteria is higher. A proper name for BII has yet to be created.
Abdominal migraine(AM) is a functional disorder that usually manifests in childhood and adolescence, without a clear pathologic mechanism or biochemical irregularity. Children frequently experience sporadic episodes of excruciating central abdominal pain accompanied by migrainous symptoms like nausea, vomiting, severe headaches, and general pallor. Abdominal migraine can be diagnosed based on clinical criteria and the exclusion of other disorders.
References
- 1 2 3 Riviello, James J.; Rioux, Stephen D. (1993). "Hair-braiding and combing-induced syncope: A paroxysmal nonepileptic event". Journal of Epilepsy. 6 (2): 115–117. doi:10.1016/S0896-6974(05)80099-4.
- 1 2 3 Lewis, Donald; Frank, L. Matthew (1993). "Hair-grooming syncope seizures". Pediatrics. 91 (4): 836–838. doi:10.1542/peds.91.4.836. PMID 8464678.
- 1 2 Igarashi, Masanori; Boehm, Robert M; May, William N; Bornhofen, John H (1988). "Syncope associated with hair-grooming". Brain and Development. 10 (4): 249–251. doi:10.1016/S0387-7604(88)80006-8. PMID 3218704.
- ↑ Evans, W. N.; Acherman, R.; Kip, K.; Restrepo, H. (1 July 2009). "Hair-Grooming Syncope in Children". Clinical Pediatrics. 48 (8): 834–836. doi:10.1177/0009922809339204. PMID 19571334.
- ↑ "Fainting by Follicle". Pediatrics for Parents. 26 (3): 1. March 2010.