Related Research Articles

Health informatics is the study and implementation of computer structures and algorithms to improve communication, understanding, and management of medical information. It can be view as branch of engineering and applied science.

An electronic health record (EHR) is the systematized collection of patient and population electronically stored health information in a digital format. These records can be shared across different health care settings. Records are shared through network-connected, enterprise-wide information systems or other information networks and exchanges. EHRs may include a range of data, including demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal statistics like age and weight, and billing information.

Telehealth is the distribution of health-related services and information via electronic information and telecommunication technologies. It allows long-distance patient and clinician contact, care, advice, reminders, education, intervention, monitoring, and remote admissions. Telemedicine is sometimes used as a synonym, or is used in a more limited sense to describe remote clinical services, such as diagnosis and monitoring. When rural settings, lack of transport, a lack of mobility, conditions due to outbreaks, epidemics or pandemics, decreased funding, or a lack of staff restrict access to care, telehealth may bridge the gap as well as provide distance-learning; meetings, supervision, and presentations between practitioners; online information and health data management and healthcare system integration. Telehealth could include two clinicians discussing a case over video conference; a robotic surgery occurring through remote access; physical therapy done via digital monitoring instruments, live feed and application combinations; tests being forwarded between facilities for interpretation by a higher specialist; home monitoring through continuous sending of patient health data; client to practitioner online conference; or even videophone interpretation during a consult.
eHealth describes healthcare services which are supported by digital processes, communication or technology such as electronic prescribing, Telehealth, or Electronic Health Records (EHRs). The use of electronic processes in healthcare dated back to at least the 1990s. Usage of the term varies as it covers not just "Internet medicine" as it was conceived during that time, but also "virtually everything related to computers and medicine". A study in 2005 found 51 unique definitions. Some argue that it is interchangeable with health informatics with a broad definition covering electronic/digital processes in health while others use it in the narrower sense of healthcare practice using the Internet. It can also include health applications and links on mobile phones, referred to as mHealth or m-Health.
A personal health record (PHR) is a health record where health data and other information related to the care of a patient is maintained by the patient. This stands in contrast to the more widely used electronic medical record, which is operated by institutions and contains data entered by clinicians to support insurance claims. The intention of a PHR is to provide a complete and accurate summary of an individual's medical history which is accessible online. The health data on a PHR might include patient-reported outcome data, lab results, and data from devices such as wireless electronic weighing scales or from a smartphone.
Health technology is defined by the World Health Organization as the "application of organized knowledge and skills in the form of devices, medicines, vaccines, procedures, and systems developed to solve a health problem and improve quality of lives". This includes pharmaceuticals, devices, procedures, and organizational systems used in the healthcare industry, as well as computer-supported information systems. In the United States, these technologies involve standardized physical objects, as well as traditional and designed social means and methods to treat or care for patients.
An e-patient is a health consumer who participates fully in his/her medical care, primarily by gathering information about medical conditions that impact them and their families, using the Internet and other digital tools. The term encompasses those who seek guidance for their own ailments and the friends and family members who go online on their behalf. E-patients report two effects of their health research: "better health information and services, and different, but not always better, relationships with their doctors."

Gunther Eysenbach is a German-Canadian researcher on healthcare, especially health policy, eHealth, and consumer health informatics.
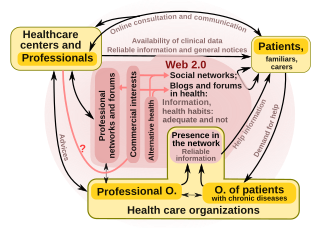
"Health 2.0" is a term introduced in the mid-2000s, as the subset of health care technologies mirroring the wider Web 2.0 movement. It has been defined variously as including social media, user-generated content, and cloud-based and mobile technologies. Some Health 2.0 proponents see these technologies as empowering patients to have greater control over their own health care and diminishing medical paternalism. Critics of the technologies have expressed concerns about possible misinformation and violations of patient privacy.

mHealth is an abbreviation for mobile health, a term used for the practice of medicine and public health supported by mobile devices. The term is most commonly used in reference to using mobile communication devices, such as mobile phones, tablet computers and personal digital assistants (PDAs), and wearable devices such as smart watches, for health services, information, and data collection. The mHealth field has emerged as a sub-segment of eHealth, the use of information and communication technology (ICT), such as computers, mobile phones, communications satellite, patient monitors, etc., for health services and information. mHealth applications include the use of mobile devices in collecting community and clinical health data, delivery/sharing of healthcare information for practitioners, researchers and patients, real-time monitoring of patient vital signs, the direct provision of care as well as training and collaboration of health workers.
Health information technology (HIT) is health technology, particularly information technology, applied to health and health care. It supports health information management across computerized systems and the secure exchange of health information between consumers, providers, payers, and quality monitors. Based on a 2008 report on a small series of studies conducted at four sites that provide ambulatory care – three U.S. medical centers and one in the Netherlands, the use of electronic health records (EHRs) was viewed as the most promising tool for improving the overall quality, safety and efficiency of the health delivery system.
Patient participation is a trend that arose in answer to medical paternalism. Informed consent is a process where patients make decisions informed by the advice of medical professionals.
Digital health is a discipline that includes digital care programs, technologies with health, healthcare, living, and society to enhance the efficiency of healthcare delivery and to make medicine more personalized and precise. It uses information and communication technologies to facilitate understanding of health problems and challenges faced by people receiving medical treatment and social prescribing in more personalised and precise ways. The definitions of digital health and its remits overlap in many ways with those of health and medical informatics.
Health information on the Internet refers to all health-related information communicated through or available on the Internet.
Infodemiology was defined by Gunther Eysenbach in the early 2000s as information epidemiology. It is an area of science research focused on scanning the internet for user-contributed health-related content, with the ultimate goal of improving public health. It is also defined as the science of mitigating public health problems resulting from an infodemic.
Health Web Science (HWS) is a sub-discipline of Web Science that examines the interplay between health sciences, health and well-being, and the World Wide Web. It assumes that each domain influences the others. HWS thus complements and overlaps with Medicine 2.0. Research has uncovered emergent properties that arise as individuals interact with each other, with healthcare providers and with the Web itself.

Dipak Kalra is President of the European Institute for Health Records and of the European Institute for Innovation through Health Data. He undertakes international research and standards development, and advises on adoption strategies, relating to Electronic Health Records.

Artificial intelligence in healthcare is a term used to describe the use of machine-learning algorithms and software, or artificial intelligence (AI), to copy human cognition in the analysis, presentation, and understanding of complex medical and health care data, or to exceed human capabilities by providing new ways to diagnose, treat, or prevent disease. Specifically, AI is the ability of computer algorithms to approximate conclusions based solely on input data.
Health data is any data "related to health conditions, reproductive outcomes, causes of death, and quality of life" for an individual or population. Health data includes clinical metrics along with environmental, socioeconomic, and behavioral information pertinent to health and wellness. A plurality of health data are collected and used when individuals interact with health care systems. This data, collected by health care providers, typically includes a record of services received, conditions of those services, and clinical outcomes or information concerning those services. Historically, most health data has been sourced from this framework. The advent of eHealth and advances in health information technology, however, have expanded the collection and use of health data—but have also engendered new security, privacy, and ethical concerns. The increasing collection and use of health data by patients is a major component of digital health.
EMRBots are experimental artificially generated electronic medical records (EMRs). The aim of EMRBots is to allow non-commercial entities to use the artificial patient repositories to practice statistical and machine-learning algorithms. Commercial entities can also use the repositories for any purpose, as long as they do not create software products using the repositories.
References
- ↑ "What is Web 3.0? Semantic Web & other Web 3.0 Concepts Explained in Plain English". Digital Inspiration. Retrieved December 10, 2011.
- ↑ "The Semantic Web". scientificamerican.com. Retrieved December 9, 2011.
- 1 2 Tony Shaw (17 August 2010). "Healthy Knowledge: Semantic Technology & the Healthcare Revolution". EContent Magazine. Retrieved December 9, 2011.
- 1 2 3 4 Nash, David B. (2008). "Health 3.0". P&T. 33 (2): 69–75. PMC 2730068 . PMID 19749994.
- ↑ Giustini, D. (2007). "Web 3.0 and medicine: make way for the semantic web". British Medical Journal . 335 (7633): 1273–1274. doi: 10.1136/bmj.39428.494236.BE . PMC 2151149 . PMID 18156223.
- ↑ "SemTech 2010 Speaks Out About Health 3.0 -- Open Healthcare Information Architecture". PRWeb. 5 May 2010.
- 1 2 Shachak A., Jadad A.R. (2010). "Electronic Health Records in the Age of Social Networks and Global Telecommunications". Journal of the American Medical Association. 303 (5): 452–453. doi:10.1001/jama.2010.63. PMID 20124543.
- ↑ Joseph F. Coughlin. "Health 3.0: Baby Boomers, Social Media & the Evolution of Digital Healing". Big Think.
- ↑ Marlene Beggelman. "Virtual Reasoning Redefining Healthcare Through Health 3.0" (PDF). Enhanced Medical Decisions Inc. Archived from the original (PDF) on 2011-08-15.
- ↑ "JMIR-Medicine 2.0: Social Networking, Collaboration, Participation, Apomediation, and Openness - Eysenbach - Journal of Medical Internet Research". Journal of Medical Internet Research.
- ↑ "Pew Research Center: Internet, Science & Technology". pewinternet.org. 8 October 2015.
- ↑ Eysenbach G, Powell J, Englesakis M, Rizo C, Stern A (2004). "Health related virtual communities and electronic support groups: systematic review of the effects of online peer to peer interactions". BMJ. 328 (7449): 1–6. doi:10.1136/bmj.328.7449.1166. PMC 411092 . PMID 15142921.
- ↑ Wang, Y. Claire; DeSalvo, Karen (2018). "Timely, Granular, and Actionable: Informatics in the Public Health 3.0 Era". American Journal of Public Health. 108 (7): 931. doi:10.2105/AJPH.2018.304406. PMC 5993377 . PMID 29771614.
- ↑ Wang, Y. Claire; DeSalvo, Karen (2018). "Timely, Granular, and Actionable: Informatics in the Public Health 3.0 Era". American Journal of Public Health. 108 (7): 932. doi:10.2105/AJPH.2018.304406. PMC 5993377 . PMID 29771614.