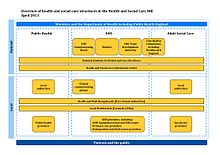
The Health and Social Care Act 2012 is an act of the Parliament of the United Kingdom. It provided for the most extensive reorganisation of the structure of the National Health Service in England to date. It removed responsibility for the health of citizens from the Secretary of State for Health, which the post had carried since the inception of the NHS in 1948. It abolished primary care trusts (PCTs) and strategic health authorities (SHAs) and transferred between £60 billion and £80 billion of "commissioning", or healthcare funds, from the abolished PCTs to several hundred clinical commissioning groups, partly run by the general practitioners (GPs) in England. A new executive agency of the Department of Health, Public Health England, was established under the act on 1 April 2013.

Clinical commissioning groups (CCGs) were NHS organisations set up by the Health and Social Care Act 2012 to organise the delivery of NHS services in each of their local areas in England. On 1 July 2022 they were abolished and replaced by Integrated care systems as a result of the Health and Care Act 2022.

NHS England, officially the NHS Commissioning Board, is an executive non-departmental public body of the Department of Health and Social Care. It oversees the budget, planning, delivery and day-to-day operation of the commissioning side of the National Health Service in England as set out in the Health and Social Care Act 2012. It directly commissions NHS general practitioners, dentists, optometrists and some specialist services. The Secretary of State publishes annually a document known as the NHS mandate which specifies the objectives which the Board should seek to achieve. National Health Service Regulations are published each year to give legal force to the mandate.
Healthcare in London, which consumes about a fifth of the NHS budget in England, is in many respects distinct from that in the rest of the United Kingdom, or England.
Healthcare in Dorset was primarily the responsibility of Dorset Clinical Commissioning Group until July 2022. Dorset County Council is leading in the development of an electronic health record, to be called the Dorset Care Record, provided by Orion Health. It is intended to enable all health and social care providers to share records.
Healthcare in Devon was the responsibility of two clinical commissioning groups until July 2022, one covering Northern, Eastern and Western Devon, and one covering South Devon and Torbay. It was announced in November 2018 that the two were to merge.
Healthcare in Worcestershire was the responsibility of three Clinical Commissioning Groups until July 2022, covering, respectively Redditch and Bromsgrove, Wyre Forest and South Worcestershire.

Healthcare in Kent has, from 1 July 2022, been mainly the responsibility of the Kent & Medway Integrated Care Board. Certain specialised services are directly commissioned by NHS England, coordinated through the South East integrated regional team. Some NHS England structures are aligned on a Kent and Medway basis, others on a South East basis and there is liaison with London to provide many tertiary healthcare services.
Healthcare in Bedfordshire is the responsibility of Bedfordshire and Luton Integrated Care Systems.
Healthcare in Somerset, England was the responsibility of three clinical commissioning groups (CCGs) until July 2022. These covered the ceremonial county of Somerset, which comprises the areas governed by Somerset County Council and the unitary authorities of North Somerset and Bath and North East Somerset.
Healthcare in Sussex was the responsibility of seven Clinical Commissioning Groups covering: Brighton and Hove; Coastal West Sussex; Horsham and Mid Sussex; Crawley; Eastbourne Hailsham and Seaford; Hastings and Rother; High Weald; and Lewes-Havens from 2013 to 2020. From April 2020 they were merged into three covering East Sussex, West Sussex, and Brighton and Hove.
Healthcare in Staffordshire was the responsibility of six clinical commissioning groups until July 2022, covering Stafford & Surrounds, North Staffordshire, South East Staffordshire and Seisdon Peninsula, East Staffordshire, Cannock Chase, and Stoke-on-Trent.
Healthcare in Cornwall, United Kingdom, was, until July 2022, the responsibility of Kernow clinical commissioning group, a National Health Service (NHS) organisation set up by the Health and Social Care Act 2012 to organise the delivery of NHS services in England. As far as the NHS is concerned, Cornwall includes the Isles of Scilly.
The "Greater Manchester Model" of NHS health care was a system uniquely devolved within England, by way of close integration with the Greater Manchester Combined Authority and local authorities, led by the Mayor of Greater Manchester. In July 2022 the Greater Manchester integrated care system took over responsibility for health and social care in the conurbation. The financial plan for 2022-23 had an initial shortage of £187 million.
Healthcare in Essex is now the responsibility of six clinical commissioning groups: Basildon and Brentwood, Mid Essex, North East Essex, Southend, Thurrock and West Essex.
Healthcare in Northumberland was the responsibility of the Northumberland, Newcastle Gateshead, and North Tyneside clinical commissioning groups from 2013 to 2022 before being replaced by integrated care systems.
Healthcare in Leicestershire was the responsibility of three clinical commissioning groups covering West Leicestershire, Leicester City and East Leicestershire and Rutland until July 2022. As far as the NHS is concerned Rutland is generally treated as part of Leicestershire.
Healthcare in Northamptonshire was the responsibility of Northamptonshire Clinical Commissioning Group until July 2022, with some involvement of Cambridgeshire and Peterborough CCG.
Healthcare in Norfolk was the responsibility of five clinical commissioning groups: Great Yarmouth and Waveney CCG, Norwich CCG, North Norfolk CCG, West Norfolk CCG and South Norfolk CCG, they merged in April 2020 becoming the Norfolk and Waveney CCG until they were replaced by an integrated care system in July 2022. Social Care is the responsibility of Norfolk County Council.
United Kingdom health law concerns the laws in the United Kingdom concerning health care and medicine, primarily administered through the National Health Service.