Diffusing capacity of the lung (DL) measures the transfer of gas from air in the lung, to the red blood cells in lung blood vessels. It is part of a comprehensive series of pulmonary function tests to determine the overall ability of the lung to transport gas into and out of the blood. DL, especially DLCO, is reduced in certain diseases of the lung and heart. DLCO measurement has been standardized according to a position paper by a task force of the European Respiratory and American Thoracic Societies.
Dead space is the volume of air that is inhaled that does not take part in the gas exchange, because it either remains in the conducting airways or reaches alveoli that are not perfused or poorly perfused. It means that not all the air in each breath is available for the exchange of oxygen and carbon dioxide. Mammals breathe in and out of their lungs, wasting that part of the inhalation which remains in the conducting airways where no gas exchange can occur.

Lung volumes and lung capacities refer to the volume of air in the lungs at different phases of the respiratory cycle.
Gas exchange is the physical process by which gases move passively by diffusion across a surface. For example, this surface might be the air/water interface of a water body, the surface of a gas bubble in a liquid, a gas-permeable membrane, or a biological membrane that forms the boundary between an organism and its extracellular environment.

A spirometer is an apparatus for measuring the volume of air inspired and expired by the lungs. A spirometer measures ventilation, the movement of air into and out of the lungs. The spirogram will identify two different types of abnormal ventilation patterns, obstructive and restrictive. There are various types of spirometers that use a number of different methods for measurement.

Hypercapnia (from the Greek hyper = "above" or "too much" and kapnos = "smoke"), also known as hypercarbia and CO2 retention, is a condition of abnormally elevated carbon dioxide (CO2) levels in the blood. Carbon dioxide is a gaseous product of the body's metabolism and is normally expelled through the lungs. Carbon dioxide may accumulate in any condition that causes hypoventilation, a reduction of alveolar ventilation (the clearance of air from the small sacs of the lung where gas exchange takes place) as well as resulting from inhalation of CO2. Inability of the lungs to clear carbon dioxide, or inhalation of elevated levels of CO2, leads to respiratory acidosis. Eventually the body compensates for the raised acidity by retaining alkali in the kidneys, a process known as "metabolic compensation".

Spirometry is the most common of the pulmonary function tests (PFTs). It measures lung function, specifically the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is helpful in assessing breathing patterns that identify conditions such as asthma, pulmonary fibrosis, cystic fibrosis, and COPD. It is also helpful as part of a system of health surveillance, in which breathing patterns are measured over time.

A plethysmograph is an instrument for measuring changes in volume within an organ or whole body. The word is derived from the Greek "plethysmos", and "graphein".
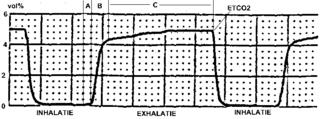
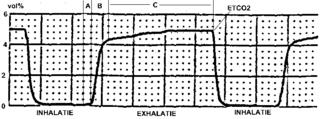
Capnography is the monitoring of the concentration or partial pressure of carbon dioxide (CO
2) in the respiratory gases. Its main development has been as a monitoring tool for use during anesthesia and intensive care. It is usually presented as a graph of CO
2 (measured in kilopascals, "kPa" or millimeters of mercury, "mmHg") plotted against time, or, less commonly, but more usefully, expired volume (known as volumetric capnography). The plot may also show the inspired CO
2, which is of interest when rebreathing systems are being used. When the measurement is taken at the end of a breath (exhaling), it is called "end tidal" CO
2 (PETCO2).
The method of standard addition is a type of quantitative analysis approach often used in analytical chemistry whereby the standard is added directly to the aliquots of analyzed sample. This method is used in situations where sample matrix also contributes to the analytical signal, a situation known as the matrix effect, thus making it impossible to compare the analytical signal between sample and standard using the traditional calibration curve approach.

Functional residual capacity (FRC) is the volume of air present in the lungs at the end of passive expiration. At FRC, the opposing elastic recoil forces of the lungs and chest wall are in equilibrium and there is no exertion by the diaphragm or other respiratory muscles.
High-frequency ventilation is a type of mechanical ventilation which utilizes a respiratory rate greater than four times the normal value. and very small tidal volumes. High frequency ventilation is thought to reduce ventilator-associated lung injury (VALI), especially in the context of ARDS and acute lung injury. This is commonly referred to as lung protective ventilation. There are different types of high-frequency ventilation. Each type has its own unique advantages and disadvantages. The types of HFV are characterized by the delivery system and the type of exhalation phase.

Pulmonary function testing (PFT) is a complete evaluation of the respiratory system including patient history, physical examinations, and tests of pulmonary function. The primary purpose of pulmonary function testing is to identify the severity of pulmonary impairment. Pulmonary function testing has diagnostic and therapeutic roles and helps clinicians answer some general questions about patients with lung disease. PFTs are normally performed by a pulmonary function technician, respiratory therapist, respiratory physiologist, physiotherapist, pulmonologist, or general practitioner.
Nitrogen washout is a test for measuring anatomic dead space in the lung during a respiratory cycle, as well as some parameters related to the closure of airways.

A pulmonary contusion, also known as lung contusion, is a bruise of the lung, caused by chest trauma. As a result of damage to capillaries, blood and other fluids accumulate in the lung tissue. The excess fluid interferes with gas exchange, potentially leading to inadequate oxygen levels (hypoxia). Unlike pulmonary laceration, another type of lung injury, pulmonary contusion does not involve a cut or tear of the lung tissue.
Hydrostatic weighing, also referred to as underwater weighing, hydrostatic body composition analysis and hydrodensitometry, is a technique for measuring the density of a living person's body. It is a direct application of Archimedes' principle, that an object displaces its own volume of water.

Breathing is the process of moving air into and from the lungs to facilitate gas exchange with the internal environment, mostly to flush out carbon dioxide and bring in oxygen.

Indirect calorimetry calculates heat that living organisms produce by measuring either their production of carbon dioxide and nitrogen waste, or from their consumption of oxygen. Indirect calorimetry estimates the type and rate of substrate utilization and energy metabolism in vivo starting from gas exchange measurements. This technique provides unique information, is noninvasive, and can be advantageously combined with other experimental methods to investigate numerous aspects of nutrient assimilation, thermogenesis, the energetics of physical exercise, and the pathogenesis of metabolic diseases.
Work of breathing (WOB) is the energy expended to inhale and exhale a breathing gas. It is usually expressed as work per unit volume, for example, joules/litre, or as a work rate (power), such as joules/min or equivalent units, as it is not particularly useful without a reference to volume or time. It can be calculated in terms of the pulmonary pressure multiplied by the change in pulmonary volume, or in terms of the oxygen consumption attributable to breathing.
Hyperpolarized gas MRI, also known as hyperpolarized helium-3 MRI or HPHe-3 MRI, is a medical imaging technique that uses hyperpolarized gases to improve the sensitivity and spatial resolution of magnetic resonance imaging (MRI). This technique has many potential applications in medicine, including the imaging of the lungs and other areas of the body with low tissue density.