Related Research Articles

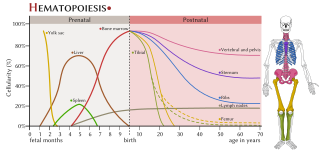
Haematopoiesis is the formation of blood cellular components. All cellular blood components are derived from haematopoietic stem cells. In a healthy adult human, roughly ten billion to a hundred billion new blood cells are produced per day, in order to maintain steady state levels in the peripheral circulation.

Bone marrow is a semi-solid tissue found within the spongy portions of bones. In birds and mammals, bone marrow is the primary site of new blood cell production. It is composed of hematopoietic cells, marrow adipose tissue, and supportive stromal cells. In adult humans, bone marrow is primarily located in the ribs, vertebrae, sternum, and bones of the pelvis. Bone marrow comprises approximately 5% of total body mass in healthy adult humans, such that a man weighing 73 kg (161 lbs) will have around 3.7 kg (8 lbs) of bone marrow.

The endothelium is a single layer of squamous endothelial cells that line the interior surface of blood vessels and lymphatic vessels. The endothelium forms an interface between circulating blood or lymph in the lumen and the rest of the vessel wall. Endothelial cells form the barrier between vessels and tissue and control the flow of substances and fluid into and out of a tissue.

Hematopoietic stem-cell transplantation (HSCT) is the transplantation of multipotent hematopoietic stem cells, usually derived from bone marrow, peripheral blood, or umbilical cord blood, in order to replicate inside a patient and produce additional normal blood cells. HSCT may be autologous, syngeneic, or allogeneic.

Hematopoietic stem cells (HSCs) are the stem cells that give rise to other blood cells. This process is called haematopoiesis. In vertebrates, the first definitive HSCs arise from the ventral endothelial wall of the embryonic aorta within the (midgestational) aorta-gonad-mesonephros region, through a process known as endothelial-to-hematopoietic transition. In adults, haematopoiesis occurs in the red bone marrow, in the core of most bones. The red bone marrow is derived from the layer of the embryo called the mesoderm.

CD34 is a transmembrane phosphoglycoprotein protein encoded by the CD34 gene in humans, mice, rats and other species.

Extramedullary hematopoiesis refers to hematopoiesis occurring outside of the medulla of the bone. It can be physiologic or pathologic.
The aorta-gonad-mesonephros (AGM) is a region of embryonic mesoderm that develops during embryonic development from the para-aortic splanchnopleura in chick, mouse and human embryos. The very first adult definitive haematopoietic stem cells, capable of long-term multilineage repopulation of adult irradiated recipients, originate from the ventral endothelial wall of the embryonic dorsal aorta, through an endothelial transdifferentiation process referred to as an 'endothelial-to-haematopoietic transition' (EHT). In the mouse embryo, these very first HSCs are characterised by their expression of Ly6A-GFP (Sca1), CD31, CD34, cKit, CD27, CD41, Gata2, Runx1, Notch1, and BMP amongst others.
Hemangioblasts are the multipotent precursor cells that can differentiate into both hematopoietic and endothelial cells. In the mouse embryo, the emergence of blood islands in the yolk sac at embryonic day 7 marks the onset of hematopoiesis. From these blood islands, the hematopoietic cells and vasculature are formed shortly after. Hemangioblasts are the progenitors that form the blood islands. To date, the hemangioblast has been identified in human, mouse and zebrafish embryos.
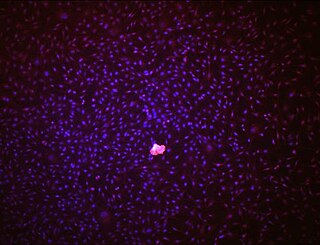
Endothelial stem cells (ESCs) are one of three types of stem cells found in bone marrow. They are multipotent, which describes the ability to give rise to many cell types, whereas a pluripotent stem cell can give rise to all types. ESCs have the characteristic properties of a stem cell: self-renewal and differentiation. These parent stem cells, ESCs, give rise to progenitor cells, which are intermediate stem cells that lose potency. Progenitor stem cells are committed to differentiating along a particular cell developmental pathway. ESCs will eventually produce endothelial cells (ECs), which create the thin-walled endothelium that lines the inner surface of blood vessels and lymphatic vessels. The blood vessels include arteries and veins. Endothelial cells can be found throughout the whole vascular system and they also play a vital role in the movement of white blood cells

Granulopoiesis is a part of haematopoiesis, that leads to the production of granulocytes. A granulocyte, also referred to as a polymorphonuclear leukocyte (PMN), is a type of white blood cell that has multi lobed nuclei, usually containing three lobes, and has a significant amount of cytoplasmic granules within the cell. Granulopoiesis takes place in the bone marrow. It leads to the production of three types of mature granulocytes: neutrophils, eosinophils and basophils.
Endothelial progenitor cell is a term that has been applied to multiple different cell types that play roles in the regeneration of the endothelial lining of blood vessels. Outgrowth endothelial cells are an EPC subtype committed to endothelial cell formation. Despite the history and controversy, the EPC in all its forms remains a promising target of regenerative medicine research.

Fms-related tyrosine kinase 3 ligand (FLT3LG) is a protein which in humans is encoded by the FLT3LG gene.
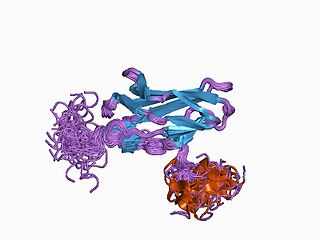
Runt-related transcription factor 1 (RUNX1) also known as acute myeloid leukemia 1 protein (AML1) or core-binding factor subunit alpha-2 (CBFA2) is a protein that in humans is encoded by the RUNX1 gene.

GATA2 or GATA-binding factor 2 is a transcription factor, i.e. a nuclear protein which regulates the expression of genes. It regulates many genes that are critical for the embryonic development, self-renewal, maintenance, and functionality of blood-forming, lympathic system-forming, and other tissue-forming stem cells. GATA2 is encoded by the GATA2 gene, a gene which often suffers germline and somatic mutations which lead to a wide range of familial and sporadic diseases, respectively. The gene and its product are targets for the treatment of these diseases.
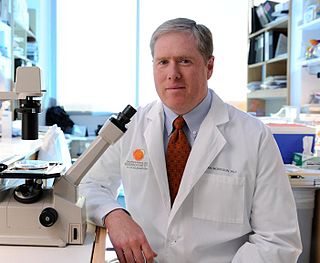
Sean J. Morrison is a Canadian-American stem cell biologist and cancer researcher. Morrison is the director of Children's Medical Center Research Institute at UT Southwestern (CRI), a nonprofit research institute established in 2011 as a joint venture between Children’s Health System of Texas and UT Southwestern Medical Center. With Morrison as founding director, CRI was established to perform transformative biomedical research at the interface of stem cell biology, cancer and metabolism to better understand the biological basis of disease. He is a Howard Hughes Medical Institute Investigator, has served as president of the International Society for Stem Cell Research, and is a member of the U.S. National Academy of Medicine, U.S. National Academy of Sciences and European Molecular Biology Organization.
Hepatic veno-occlusive disease (VOD) or veno-occlusive disease with immunodeficiency is a potentially life-threatening condition in which some of the small veins in the liver are obstructed. It is a complication of high-dose chemotherapy given before a bone marrow transplant and/or excessive exposure to hepatotoxic pyrrolizidine alkaloids. It is classically marked by weight gain due to fluid retention, increased liver size, and raised levels of bilirubin in the blood. The name sinusoidal obstruction syndrome (SOS) is preferred if hepatic veno-occlusive disease happens as a result of chemotherapy or bone marrow transplantation.
The haematopoietic system is the system in the body involved in the creation of the cells of blood.
Many human blood cells, such as red blood cells (RBCs), immune cells, and even platelets all originate from the same progenitor cell, the hematopoietic stem cell (HSC). As these cells are short-lived, there needs to be a steady turnover of new blood cells and the maintenance of an HSC pool. This is broadly termed hematopoiesis. This event requires a special environment, termed the hematopoietic stem cell niche, which provides the protection and signals necessary to carry out the differentiation of cells from HSC progenitors. This stem-cell niche relocates from the yolk sac to eventually rest in the bone marrow of mammals. Many pathological states can arise from disturbances in this niche environment, highlighting its importance in maintaining hematopoiesis.
AI-10-49 is a small molecule inhibitor of leukemic oncoprotein CBFβ-SMHHC developed by the laboratory of John Bushweller with efficacy demonstrated by the laboratories of Lucio H. Castilla and Monica Guzman. AI-10-49 allosterically binds to CBFβ-SMMHC and disrupts protein-protein interaction between CBFβ-SMMHC and tumor suppressor RUNX1. This inhibitor is under development as an anti-leukemic drug.
References
- 1 2 Yoshimoto, M; Yoder, MC (12 February 2009). "Developmental biology: Birth of the blood cell". Nature. 457 (7231): 801–3. doi:10.1038/457801a. PMID 19212393.
- ↑ Swiers, G; Rode, C; Azzoni, E; de Bruijn, MF (December 2013). "A short history of hemogenic endothelium". Blood cells, molecules & diseases. 51 (4): 206–12. doi:10.1016/j.bcmd.2013.09.005. PMID 24095001.
- ↑ Lancrin, C; Sroczynska, P; Stephenson, C; Allen, T; Kouskoff, V; Lacaud, G (12 February 2009). "The haemangioblast generates haematopoietic cells through a haemogenic endothelium stage". Nature. 457 (7231): 892–5. doi:10.1038/nature07679. PMID 19182774.