Related Research Articles

Tuberculosis (TB), also known as the "white death", or historically as consumption, is an infectious disease usually caused by Mycobacterium tuberculosis (MTB) bacteria. Tuberculosis generally affects the lungs, but it can also affect other parts of the body. Most infections show no symptoms, in which case it is known as latent tuberculosis. Around 10% of latent infections progress to active disease which, if left untreated, kill about half of those affected. Typical symptoms of active TB are chronic cough with blood-containing mucus, fever, night sweats, and weight loss. Infection of other organs can cause a wide range of symptoms.

Staphylococcus aureus is a Gram-positive spherically shaped bacterium, a member of the Bacillota, and is a usual member of the microbiota of the body, frequently found in the upper respiratory tract and on the skin. It is often positive for catalase and nitrate reduction and is a facultative anaerobe that can grow without the need for oxygen. Although S. aureus usually acts as a commensal of the human microbiota, it can also become an opportunistic pathogen, being a common cause of skin infections including abscesses, respiratory infections such as sinusitis, and food poisoning. Pathogenic strains often promote infections by producing virulence factors such as potent protein toxins, and the expression of a cell-surface protein that binds and inactivates antibodies. S. aureus is one of the leading pathogens for deaths associated with antimicrobial resistance and the emergence of antibiotic-resistant strains, such as methicillin-resistant S. aureus (MRSA), is a worldwide problem in clinical medicine. Despite much research and development, no vaccine for S. aureus has been approved.

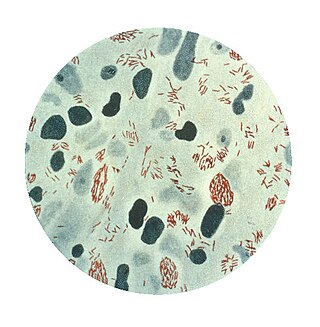
Mycobacterium tuberculosis, also known as Koch's bacillus, is a species of pathogenic bacteria in the family Mycobacteriaceae and the causative agent of tuberculosis. First discovered in 1882 by Robert Koch, M. tuberculosis has an unusual, waxy coating on its cell surface primarily due to the presence of mycolic acid. This coating makes the cells impervious to Gram staining, and as a result, M. tuberculosis can appear weakly Gram-positive. Acid-fast stains such as Ziehl–Neelsen, or fluorescent stains such as auramine are used instead to identify M. tuberculosis with a microscope. The physiology of M. tuberculosis is highly aerobic and requires high levels of oxygen. Primarily a pathogen of the mammalian respiratory system, it infects the lungs. The most frequently used diagnostic methods for tuberculosis are the tuberculin skin test, acid-fast stain, culture, and polymerase chain reaction.

Mycobacterium is a genus of over 190 species in the phylum Actinomycetota, assigned its own family, Mycobacteriaceae. This genus includes pathogens known to cause serious diseases in mammals, including tuberculosis and leprosy in humans. The Greek prefix myco- means 'fungus', alluding to this genus' mold-like colony surfaces. Since this genus has cell walls with a waxy lipid-rich outer layer that contains high concentrations of mycolic acid, acid-fast staining is used to emphasize their resistance to acids, compared to other cell types.
Mycobacterium leprae is one of the two species of bacteria that cause Hansen’s disease (leprosy), a chronic but curable infectious disease that damages the peripheral nerves and targets the skin, eyes, nose, and muscles.
Coinfection is the simultaneous infection of a host by multiple pathogen species. In virology, coinfection includes simultaneous infection of a single cell by two or more virus particles. An example is the coinfection of liver cells with hepatitis B virus and hepatitis D virus, which can arise incrementally by initial infection followed by superinfection.

Mycobacterium bovis is a slow-growing aerobic bacterium and the causative agent of tuberculosis in cattle. It is related to Mycobacterium tuberculosis, the bacterium which causes tuberculosis in humans. M. bovis can jump the species barrier and cause tuberculosis-like infection in humans and other mammals.

Rifampicin, also known as rifampin, is an ansamycin antibiotic used to treat several types of bacterial infections, including tuberculosis (TB), Mycobacterium avium complex, leprosy, and Legionnaires' disease. It is almost always used together with other antibiotics with two notable exceptions: when given as a "preferred treatment that is strongly recommended" for latent TB infection; and when used as post-exposure prophylaxis to prevent Haemophilus influenzae type b and meningococcal disease in people who have been exposed to those bacteria. Before treating a person for a long period of time, measurements of liver enzymes and blood counts are recommended. Rifampicin may be given either by mouth or intravenously.

An opportunistic infection is an infection caused by pathogens that take advantage of an opportunity not normally available. These opportunities can stem from a variety of sources, such as a weakened immune system, an altered microbiome, or breached integumentary barriers. Many of these pathogens do not necessarily cause disease in a healthy host that has a non-compromised immune system, and can, in some cases, act as commensals until the balance of the immune system is disrupted. Opportunistic infections can also be attributed to pathogens which cause mild illness in healthy individuals but lead to more serious illness when given the opportunity to take advantage of an immunocompromised host.

Plasmodium knowlesi is a parasite that causes malaria in humans and other primates. It is found throughout Southeast Asia, and is the most common cause of human malaria in Malaysia. Like other Plasmodium species, P. knowlesi has a life cycle that requires infection of both a mosquito and a warm-blooded host. While the natural warm-blooded hosts of P. knowlesi are likely various Old World monkeys, humans can be infected by P. knowlesi if they are fed upon by infected mosquitoes. P. knowlesi is a eukaryote in the phylum Apicomplexa, genus Plasmodium, and subgenus Plasmodium. It is most closely related to the human parasite Plasmodium vivax as well as other Plasmodium species that infect non-human primates.
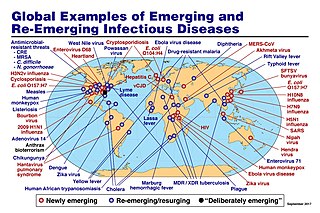
An emerging infectious disease (EID) is an infectious disease whose incidence has increased recently, and could increase in the near future. The minority that are capable of developing efficient transmission between humans can become major public and global concerns as potential causes of epidemics or pandemics. Their many impacts can be economic and societal, as well as clinical. EIDs have been increasing steadily since at least 1940.

A subclinical infection—sometimes called a preinfection or inapparent infection—is an infection by a pathogen that causes few or no signs or symptoms of infection in the host. Subclinical infections can occur in both humans and animals. Depending on the pathogen, which can be a virus or intestinal parasite, the host may be infectious and able to transmit the pathogen without ever developing symptoms; such a host is called an asymptomatic carrier. Many pathogens, including HIV, typhoid fever, and coronaviruses such as COVID-19 spread in their host populations through subclinical infection.
Mycobacterium canettii, a novel pathogenic taxon of the Mycobacterium tuberculosis complex (MTBC), was first reported in 1969 by the French microbiologist Georges Canetti, for whom the organism has been named. It formed smooth and shiny colonies, which is highly exceptional for the MTBC. It was described in detail in 1997 on the isolation of a new strain from a 2-year-old Somali patient with lymphadenitis. It did not differ from Mycobacterium tuberculosis in the biochemical tests and in its 16S rRNA sequence. It had shorter generation time than clinical isolates of M. tuberculosis and presented a unique, characteristic phenolic glycolipid and lipo-oligosaccharide. In 1998, Pfyffer described abdominal lymphatic TB in a 56-year-old Swiss man with HIV infection who lived in Kenya. Tuberculosis caused by M. canettii appears to be an emerging disease in the Horn of Africa. A history of a stay to the region should induce the clinician to consider this organism promptly even if the clinical features of TB caused by M. canettii are not specific. The natural reservoir, host range, and mode of transmission of the organism are still unknown.
A reverse zoonosis, also known as a zooanthroponosis or anthroponosis, is a pathogen reservoired in humans that is capable of being transmitted to non-human animals.

In enzymology, a β-ketoacyl-[acyl-carrier-protein] synthase III (EC 2.3.1.180) is an enzyme that catalyzes the chemical reaction

In molecular biology, hemagglutinins are receptor-binding membrane fusion glycoproteins produced by viruses in the Paramyxoviridae and Orthomyxoviridae families. Hemagglutinins are responsible for binding to receptors on red blood cells to initiate viral attachment and infection. The agglutination of red cells occurs when antibodies on one cell bind to those on others, causing amorphous aggregates of clumped cells.
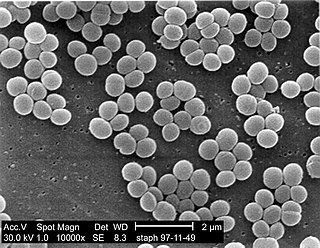
Staphylococcus is a genus of Gram-positive bacteria in the family Staphylococcaceae from the order Bacillales. Under the microscope, they appear spherical (cocci), and form in grape-like clusters. Staphylococcus species are facultative anaerobic organisms.
Staphylococcus schleiferi is a Gram-positive, cocci-shaped bacterium of the family Staphylococcaceae. It is facultatively anaerobic, coagulase-variable, and can be readily cultured on blood agar where the bacterium tends to form opaque, non-pigmented colonies and beta (β) hemolysis. There exists two subspecies under the species S. schleiferi: Staphylococcus schleiferi subsp. schleiferi and Staphylococcus schleiferi subsp. coagulans.
Staphylococcus pseudintermedius is a gram positive coccus bacteria of the genus Staphylococcus found worldwide. It is primarily a pathogen for domestic animals, but has been known to affect humans as well. S. pseudintermedius is an opportunistic pathogen that secretes immune modulating virulence factors, has many adhesion factors, and the potential to create biofilms, all of which help to determine the pathogenicity of the bacterium. Diagnoses of Staphylococcus pseudintermedius have traditionally been made using cytology, plating, and biochemical tests. More recently, molecular technologies like MALDI-TOF, DNA hybridization and PCR have become preferred over biochemical tests for their more rapid and accurate identifications. This includes the identification and diagnosis of antibiotic resistant strains.
Teixobactin is a peptide-like secondary metabolite of some species of bacteria, that kills some gram-positive bacteria. It appears to belong to a new class of antibiotics, and harms bacteria by binding to lipid II and lipid III, important precursor molecules for forming the cell wall.
References
- ↑ Michel, A.L.; Huchzermeyer, H.F.A.K. (1998). "The zoonotic importance of Mycobacterium tuberculosis : Transmission from human to monkey : Case report". Journal of the South African Veterinary Association. 69 (2): 64–5. doi: 10.4102/jsava.v69i2.819 . PMID 9760401.
- ↑ Jones-Engel, Lisa; Engel, Gregory A.; Schillaci, Michael A.; Babo, Rosnany; Froehlich, Jeffery (2001). "Detection of antibodies to selected human pathogens among wild and pet macaques (Macaca tonkeana) in Sulawesi, Indonesia". American Journal of Primatology. 54 (3): 171–178. doi: 10.1002/ajp.1021 . PMID 11443632. S2CID 21092878.
- ↑ Schillaci, M. A.; Jones-Engel, L.; Engel, G. A.; Kyes, R. C. (2006). "Exposure to human respiratory viruses among urban performing monkeys in Indonesia". The American Journal of Tropical Medicine and Hygiene. 75 (4): 716–9. doi: 10.4269/ajtmh.2006.75.716 . PMID 17038700.
- ↑ Schaumburg, Frieder; Pauly, Maude; Anoh, Etile; Mossoun, Arsene; Wiersma, Lidewij; Schubert, Grit; Flammen, Arnaud; Alabi, Abraham S.; Muyembe-Tamfum, Jean-Jacques; Grobusch, Martin P.; Karhemere, Stomy; Akoua-Koffi, Chantal; Couacy-Hymann, Emmanuel; Kremsner, Peter G.; Mellmann, Alexander; Becker, Karsten; Leendertz, Fabian H.; Peters, Georg (2015). "Staphylococcus aureus complex from animals and humans in three remote African regions". Clinical Microbiology and Infection. 21 (4): 345.e1–345.e8. doi: 10.1016/j.cmi.2014.12.001 . PMID 25596779.
- ↑ Senghore, Madikay; Bayliss, Sion C.; Kwambana-Adams, Brenda A.; Foster-Nyarko, Ebenezer; Manneh, Jainaba; Dione, Michel; Badji, Henry; Ebruke, Chinelo; Doughty, Emma L.; Thorpe, Harry A.; Jasinska, Anna J.; Schmitt, Christopher A.; Cramer, Jennifer D.; Turner, Trudy R.; Weinstock, George; Freimer, Nelson B.; Pallen, Mark J.; Feil, Edward J.; Antonio, Martin (2016). "Transmission of Staphylococcus aureus from Humans to Green Monkeys in the Gambia as Revealed by Whole-Genome Sequencing". Applied and Environmental Microbiology. 82 (19): 5910–5917. Bibcode:2016ApEnM..82.5910S. doi: 10.1128/AEM.01496-16 . PMC 5038045 . PMID 27474712.
- ↑ Rodrigues, Priscila T.; Valdivia, Hugo O.; De Oliveira, Thais C.; Alves, João Marcelo P.; Duarte, Ana Maria R. C.; Cerutti-Junior, Crispim; Buery, Julyana C.; Brito, Cristiana F. A.; De Souza, Júlio César; Hirano, Zelinda M. B.; Bueno, Marina G.; Catão-Dias, José Luiz; Malafronte, Rosely S.; Ladeia-Andrade, Simone; Mita, Toshihiro; Santamaria, Ana Maria; Calzada, José E.; Tantular, Indah S.; Kawamoto, Fumihiko; Raijmakers, Leonie R. J.; Mueller, Ivo; Pacheco, M. Andreina; Escalante, Ananias A.; Felger, Ingrid; Ferreira, Marcelo U. (2018). "Human migration and the spread of malaria parasites to the New World". Scientific Reports. 8 (1): 1993. Bibcode:2018NatSR...8.1993R. doi: 10.1038/s41598-018-19554-0 . PMC 5792595 . PMID 29386521.
- ↑ Obaldía, Nicanor; Nuñez, Marlon; Montilla, Santiago; Otero, William; Marin, Jose Camilo (2018). "Tuberculosis (TB) outbreak in a closed Aotus monkey breeding colony: Epidemiology, diagnosis and TB screening using antibody and interferon-gamma release testing". Comparative Immunology, Microbiology and Infectious Diseases. 58: 1–10. doi: 10.1016/j.cimid.2018.06.007 . PMID 30245044. S2CID 52335531.