Related Research Articles

The cervix or cervix uteri is the lower part of the uterus (womb) in the human female reproductive system. The cervix is usually 2 to 3 cm long and roughly cylindrical in shape, which changes during pregnancy. The narrow, central cervical canal runs along its entire length, connecting the uterine cavity and the lumen of the vagina. The opening into the uterus is called the internal os, and the opening into the vagina is called the external os. The lower part of the cervix, known as the vaginal portion of the cervix, bulges into the top of the vagina. The cervix has been documented anatomically since at least the time of Hippocrates, over 2,000 years ago.
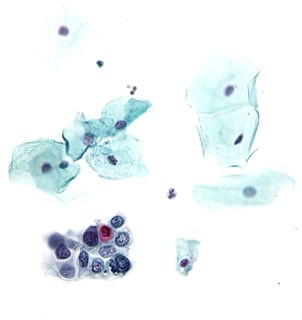
The Papanicolaou test is a method of cervical screening used to detect potentially precancerous and cancerous processes in the cervix or colon. Abnormal findings are often followed up by more sensitive diagnostic procedures and, if warranted, interventions that aim to prevent progression to cervical cancer. The test was independently invented in the 1920s by Georgios Papanikolaou and Aurel Babeș and named after Papanikolaou. A simplified version of the test was introduced by Anna Marion Hilliard in 1957.

Cervical cancer is a cancer arising from the cervix. It is due to the abnormal growth of cells that have the ability to invade or spread to other parts of the body. Early on, typically no symptoms are seen. Later symptoms may include abnormal vaginal bleeding, pelvic pain or pain during sexual intercourse. While bleeding after sex may not be serious, it may also indicate the presence of cervical cancer.

Cancer is a group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body. These contrast with benign tumors, which do not spread. Possible signs and symptoms include a lump, abnormal bleeding, prolonged cough, unexplained weight loss, and a change in bowel movements. While these symptoms may indicate cancer, they can also have other causes. Over 100 types of cancers affect humans.
Human papillomavirus infection is caused by a DNA virus from the Papillomaviridae family. Many HPV infections cause no symptoms and 90% resolve spontaneously within two years. In some cases, an HPV infection persists and results in either warts or precancerous lesions. These lesions, depending on the site affected, increase the risk of cancer of the cervix, vulva, vagina, penis, anus, mouth, tonsils, or throat. Nearly all cervical cancer is due to HPV and two strains – HPV16 and HPV18 – account for 70% of cases. HPV16 is responsible for almost 90% of HPV-positive oropharyngeal cancers. Between 60% and 90% of the other cancers listed above are also linked to HPV. HPV6 and HPV11 are common causes of genital warts and laryngeal papillomatosis.

Colposcopy is a medical diagnostic procedure to visually examine the cervix as well as the vagina and vulva using a colposcope.

Oral cancer, also known as mouth cancer, is cancer of the lining of the lips, mouth, or upper throat. In the mouth, it most commonly starts as a painless white patch, that thickens, develops red patches, an ulcer, and continues to grow. When on the lips, it commonly looks like a persistent crusting ulcer that does not heal, and slowly grows. Other symptoms may include difficult or painful swallowing, new lumps or bumps in the neck, a swelling in the mouth, or a feeling of numbness in the mouth or lips.

Anal cancer is a cancer which arises from the anus, the distal opening of the gastrointestinal tract. Symptoms may include bleeding from the anus or a lump near the anus. Other symptoms may include pain, itchiness, or discharge from the anus. A change in bowel movements may also occur.
Women's health differs from that of men in many unique ways. Women's health is an example of population health, where health is defined by the World Health Organization as "a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity". Often treated as simply women's reproductive health, many groups argue for a broader definition pertaining to the overall health of women, better expressed as "The health of women". These differences are further exacerbated in developing countries where women, whose health includes both their risks and experiences, are further disadvantaged.

Cervical intraepithelial neoplasia (CIN), also known as cervical dysplasia, is the abnormal growth of cells on the surface of the cervix that could potentially lead to cervical cancer. More specifically, CIN refers to the potentially precancerous transformation of cells of the cervix.

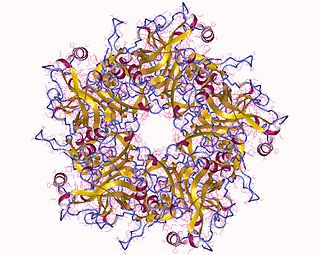
Human papillomavirus (HPV) vaccines are vaccines that prevent infection by certain types of human papillomavirus (HPV). Available HPV vaccines protect against either two, four, or nine types of HPV. All HPV vaccines protect against at least HPV types 16 and 18, which cause the greatest risk of cervical cancer. It is estimated that HPV vaccines may prevent 70% of cervical cancer, 80% of anal cancer, 60% of vaginal cancer, 40% of vulvar cancer, and show more than 90% efficacy in preventing HPV-positive oropharyngeal cancers. They additionally prevent some genital warts, with the quadrivalent and nonavalent vaccines that protect against HPV types HPV-6 and HPV-11 providing greater protection.

Ian Hector Frazer is a Scottish-born Australian immunologist, the founding CEO and Director of Research of the Translational Research Institute (Australia). Frazer and Jian Zhou developed and patented the basic technology behind the HPV vaccine against cervical cancer at the University of Queensland. Researchers at the National Cancer Institute, Georgetown University, and University of Rochester also contributed to the further development of the cervical cancer vaccine in parallel.

Gardasil is an HPV vaccine for use in the prevention of certain strains of human papillomavirus (HPV). It was developed by Merck & Co. High-risk human papilloma virus (hr-HPV) genital infection is the most common sexually transmitted infection among women. The HPV strains that Gardasil protects against are sexually transmitted, specifically HPV types 6, 11, 16 and 18. HPV types 16 and 18 cause an estimated 70% of cervical cancers, and are responsible for most HPV-induced anal, vulvar, vaginal, and penile cancer cases. HPV types 6 and 11 cause an estimated 90% of genital warts cases. HPV type 16 is responsible for almost 90% of HPV-positive oropharyngeal cancers, and the prevalence is higher in males than females. Though Gardasil does not treat existing infection, vaccination is still recommended for HPV-positive individuals, as it may protect against one or more different strains of the disease.
Vaginal cancer is an extraordinarily rare form of cancer that develops in the tissue of the vagina. Primary vaginal cancer originates from the vaginal tissue – most frequently squamous cell carcinoma, but primary vaginal adenocarcinoma, sarcoma, and melanoma have also been reported – while secondary vaginal cancer involves the metastasis of a cancer that originated in a different part of the body. Secondary vaginal cancer is more common. Signs of vaginal cancer may include abnormal vaginal bleeding, dysuria, tenesmus, or pelvic pain, though as many as 20% of women diagnosed with vaginal cancer are asymptomatic at the time of diagnosis. Vaginal cancer occurs more frequently in women over age 50, and the mean age of diagnosis of vaginal cancer is 60 years. It often can be cured if found and treated in early stages. Surgery alone or surgery combined with pelvic radiation is typically used to treat vaginal cancer.
Gynecologic oncology is a specialized field of medicine that focuses on cancers of the female reproductive system, including ovarian cancer, uterine cancer, vaginal cancer, cervical cancer, and vulvar cancer. As specialists, they have extensive training in the diagnosis and treatment of these cancers.
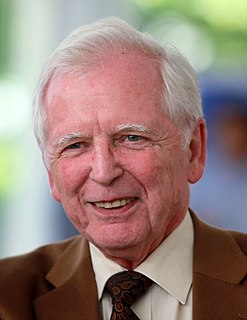
Harald zur Hausen NAS EASA APS is a German virologist and professor emeritus. He has done research on cervical cancer and discovered the role of papilloma viruses in cervical cancer, for which he received the Nobel Prize in Physiology or Medicine 2008.

Cancer screening aims to detect cancer before symptoms appear. This may involve blood tests, urine tests, DNA tests, other tests, or medical imaging. The benefits of screening in terms of cancer prevention, early detection and subsequent treatment must be weighed against any harms.

Cervical screening is the process of detecting and removing abnormal tissue or cells in the cervix before cervical cancer develops. By aiming to detect and treat cervical neoplasia early on, cervical screening aims at secondary prevention of cervical cancer. Primary prevention of cervical cancer is vaccination against HPV. Several screening methods for cervical cancer are the Pap test, liquid-based cytology, the HPV DNA testing and the visual inspection with acetic acid. Pap test and liquid-based cytology have been effective in diminishing incidence and mortality rates of cervical cancer in developed countries but not in developing countries. Prospective screening methods that can be used in low-resource areas in developing countries are the HPV DNA testing and the visual inspection. There are wide disparities in cervical screening rates and outcomes, with about 90% of deaths from cervical cancer in 2018 occurring in low and middle-income countries. To help coordinate resources to address this gap, the World Health Organization in 2020 adopted the Global Strategy for Cervical Cancer Elimination. This created the goal of vaccinating 90% of women against HPV by age 15, screening 70% of women by age 35 and again by age 45, and treating and managing 90% of patients with pre-cancer and invasive cancer, respectively.

Healthcare in Nicaragua involves the collaboration of private and public institutions. Although Nicaragua's health outcomes have improved over the past few decades with the efficient utilization of resources relative to other Central American nations, it still confronts challenges responding to its population's diverse healthcare needs.

Gynecologic cancer disparities in the United States refer to differences in incidence, prevalence, and mortality from gynecologic cancers between population groups. The five main types of gynecologic cancer include cervical cancer, ovarian cancer, endometrial cancer, vaginal cancer, and vulvar cancer. For patients with these and other gynecologic malignancies within the United States, disparities across the care continuum by socioeconomic status and racial/ethnic background have been previously identified and studied. The causes behind these disparities are multifaceted and a complex interplay of systemic differences in health as well as individual patient factors such as cultural, educational, and economic barriers.
References
- ↑ Tambouret, Rosemary (June 2013). "Screening for Cervical Cancer in Low-Resource Settings in 2011". Archives of Pathology & Laboratory Medicine. 137 (6): 782–790. doi: 10.5858/arpa.2011-0695-RA . PMID 23721273.
- ↑ "AUM students travel to Peru to help fight cervical cancer". WSFA 12 News. Montgomery, Alabama. 22 July 2010. Retrieved 22 January 2019.
- ↑ Nelson, Bryn (10 June 2011). "Cytologists battle cruel killer in Peru. Volunteers take on one of the world's highest cervical cancer rates". Cancer Cytopathology. 119 (3): 141. doi: 10.1002/cncy.20169 . PMID 21671409.