Related Research Articles
Ataxia is a neurological sign consisting of lack of voluntary coordination of muscle movements that can include gait abnormality, speech changes, and abnormalities in eye movements, that indicates dysfunction of parts of the nervous system that coordinate movement, such as the cerebellum.
Dysarthria is a speech sound disorder resulting from neurological injury of the motor component of the motor–speech system and is characterized by poor articulation of phonemes. In other words, it is a condition in which problems effectively occur with the muscles that help produce speech, often making it very difficult to pronounce words. It is unrelated to problems with understanding language, although a person can have both. Any of the speech subsystems can be affected, leading to impairments in intelligibility, audibility, naturalness, and efficiency of vocal communication. Dysarthria that has progressed to a total loss of speech is referred to as anarthria. The term dysarthria is from Neo-Latin, dys- "dysfunctional, impaired" and arthr- "joint, vocal articulation".

Olivopontocerebellar atrophy (OPCA) is the degeneration of neurons in specific areas of the brain – the cerebellum, pons, and inferior olivary nucleus. OPCA is present in several neurodegenerative syndromes, including inherited and non-inherited forms of ataxia and multiple system atrophy (MSA), with which it is primarily associated.
Spinocerebellar ataxia (SCA) is a progressive, degenerative, genetic disease with multiple types, each of which could be considered a neurological condition in its own right. An estimated 150,000 people in the United States have a diagnosis of spinocerebellar ataxia at any given time. SCA is hereditary, progressive, degenerative, and often fatal. There is no known effective treatment or cure. SCA can affect anyone of any age. The disease is caused by either a recessive or dominant gene. In many cases people are not aware that they carry a relevant gene until they have children who begin to show signs of having the disorder.
Dysmetria is a lack of coordination of movement typified by the undershoot or overshoot of intended position with the hand, arm, leg, or eye. It is a type of ataxia. It can also include an inability to judge distance or scale.
Dysdiadochokinesia (DDK) is the medical term for an impaired ability to perform rapid, alternating movements. Complete inability is called adiadochokinesia. The term is from Greek δυςdys "bad", διάδοχοςdiadochos "succeeding", κίνησιςkinesis "movement".
Cerebellar ataxia is a form of ataxia originating in the cerebellum. Non-progressive congenital ataxia (NPCA) is a classical presentation of cerebral ataxias.

Spinocerebellar ataxia type 6 (SCA6) is a rare, late-onset, autosomal dominant disorder, which, like other types of SCA, is characterized by dysarthria, oculomotor disorders, peripheral neuropathy, and ataxia of the gait, stance, and limbs due to cerebellar dysfunction. Unlike other types, SCA 6 is not fatal. This cerebellar function is permanent and progressive, differentiating it from episodic ataxia type 2 (EA2) where said dysfunction is episodic. In some SCA6 families, some members show these classic signs of SCA6 while others show signs more similar to EA2, suggesting that there is some phenotypic overlap between the two disorders. SCA6 is caused by mutations in CACNA1A, a gene encoding a calcium channel α subunit. These mutations tend to be trinucleotide repeats of CAG, leading to the production of mutant proteins containing stretches of 20 or more consecutive glutamine residues; these proteins have an increased tendency to form intracellular agglomerations. Unlike many other polyglutamine expansion disorders expansion length is not a determining factor for the age that symptoms present.
The Kurtzke Expanded Disability Status Scale (EDSS) is a method of quantifying disability in multiple sclerosis. The scale has been developed by John F. Kurtzke. The EDSS is based on a neurological examination by a clinician. However, a number of versions have been developed which enable patient self-administration.
Ramsay Hunt syndrome type 1 is a rare, degenerative, neurological disorder characterized by myoclonus epilepsy, intention tremor, progressive ataxia and occasionally cognitive impairment

Cav2.1, also called the P/Q voltage-dependent calcium channel, is a calcium channel found mainly in the brain. Specifically, it is found on the presynaptic terminals of neurons in the brain and cerebellum. Cav2.1 plays an important role in controlling the release of neurotransmitters between neurons. It is composed of multiple subunits, including alpha-1, beta, alpha-2/delta, and gamma subunits. The alpha-1 subunit is the pore-forming subunit, meaning that the calcium ions flow through it. Different kinds of calcium channels have different isoforms (versions) of the alpha-1 subunit. Cav2.1 has the alpha-1A subunit, which is encoded by the CACNA1A gene. Mutations in CACNA1A have been associated with various neurologic disorders, including familial hemiplegic migraine, episodic ataxia type 2, and spinocerebellar ataxia type 6.
Bruns apraxia, or frontal ataxia, is a gait apraxia found in patients with bilateral frontal lobe disorders. It is characterised by an inability to initiate the process of walking, despite the power and coordination of the legs being normal when tested in the seated or lying position. The gait is broad-based with short steps with a tendency to fall backwards. It was originally described in patients with frontal lobe tumours, but is now more commonly seen in patients with cerebrovascular disease.
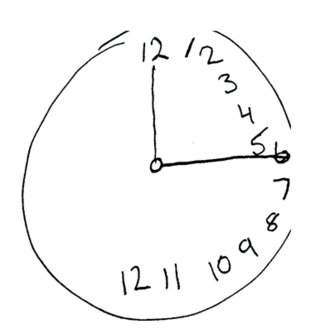
The Montreal Cognitive Assessment (MoCA) is a widely used screening assessment for detecting cognitive impairment. It was created in 1996 by Ziad Nasreddine in Montreal, Quebec. It was validated in the setting of mild cognitive impairment (MCI), and has subsequently been adopted in numerous other clinical settings. This test consists of 30 points and takes 10 minutes for the individual to complete. The original English version is performed in seven steps, which may change in some countries dependent on education and culture. The basics of this test include short-term memory, executive function, attention, focus, and more.
Dyskinetic cerebral palsy (DCP) is a subtype of cerebral palsy (CP) and is characterized by impaired muscle tone regulation, coordination and movement control. Dystonia and choreoathetosis are the two most dominant movement disorders in patients with DCP.

Harding ataxia is an autosomal recessive cerebellar ataxia originally described by Harding in 1981. This form of cerebellar ataxia is similar to Friedreich ataxia including that it results in poor reflexes and balance, but differs in several ways, including the absence of diabetes mellitus, optic atrophy, cardiomyopathy, skeletal abnormalities, and the fact that tendon reflexes in the arms and knees remain intact. This form of ataxia is characterized by onset in the first 20 years, and is less severe than Friedreich ataxia. Additional cases were diagnosed in 1989, 1990, 1991, and 1998.
Oculomotor apraxia (OMA) is the absence or defect of controlled, voluntary, and purposeful eye movement. It was first described in 1952 by the American ophthalmologist David Glendenning Cogan. People with this condition have difficulty moving their eyes horizontally and moving them quickly. The main difficulty is in saccade initiation, but there is also impaired cancellation of the vestibulo-ocular reflex. Patients have to turn their head in order to compensate for the lack of eye movement initiation in order to follow an object or see objects in their peripheral vision, but they often exceed their target. There is controversy regarding whether OMA should be considered an apraxia, since apraxia is the inability to perform a learned or skilled motor action to command, and saccade initiation is neither a learned nor a skilled action.

Autosomal dominant cerebellar ataxia (ADCA) is a form of spinocerebellar ataxia inherited in an autosomal dominant manner. ADCA is a genetically inherited condition that causes deterioration of the nervous system leading to disorder and a decrease or loss of function to regions of the body.

An upper limb neurological examination is part of the neurological examination, and is used to assess the motor and sensory neurons which supply the upper limbs. This assessment helps to detect any impairment of the nervous system, being used both as a screening and an investigative tool. The examination findings when combined with a detailed history of a patient, can help a doctor reach a specific or differential diagnosis. This would enable the doctor to commence treatment if a specific diagnosis has been made, or order further investigations if there are differential diagnoses.

Spinocerebellar ataxia type 1 (SCA1) is a rare autosomal dominant disorder, which, like other spinocerebellar ataxias, is characterized by neurological symptoms including dysarthria, hypermetric saccades, and ataxia of gait and stance. This cerebellar dysfunction is progressive and permanent. First onset of symptoms is normally between 30 and 40 years of age, though juvenile onset can occur. Death typically occurs within 10 to 30 years from onset.

Cerebellar degeneration is a condition in which cerebellar cells, otherwise known as neurons, become damaged and progressively weaken in the cerebellum. There are two types of cerebellar degeneration; paraneoplastic cerebellar degeneration, and alcoholic or nutritional cerebellar degeneration. As the cerebellum contributes to the coordination and regulation of motor activities, as well as controlling equilibrium of the human body, any degeneration to this part of the organ can be life-threatening. Cerebellar degeneration can result in disorders in fine movement, posture, and motor learning in humans, due to a disturbance of the vestibular system. This condition may not only cause cerebellar damage on a temporary or permanent basis, but can also affect other tissues of the central nervous system, those including the cerebral cortex, spinal cord and the brainstem.
References
- ↑ Schoch, B; et al. (Nov 2007). "Reliability and validity of ICARS in focal cerebellar lesions". Movement Disorders. 22 (15): 2162–2169. doi:10.1002/mds.21543. PMID 17712842.
- ↑ Schmitz-Hubsch, T; et al. (May 2006). "Reliability and validity of the International Cooperative Ataxia Rating Scale: a study in 156 spinocerebellar ataxia patients". Movement Disorders. 21 (5): 699–704. doi:10.1002/mds.20781. PMID 16450347.
- ↑ Storey, E; Tuck, K.; Hester, R.; Hughes, A.; Churchyard, A. (Feb 2004). "Inter-rater reliability of the International Cooperative Ataxia Rating Scale (ICARS)". Movement Disorders. 19 (2): 190–192. doi:10.1002/mds.10657. PMID 14978674.
- ↑ Subramony, SH (Mar 2007). "SARA - a new clinical scale for the assessment and rating of ataxia". Nature Clinical Practice Neurology. 3 (3): 136–137. doi:10.1038/ncpneuro0426. PMID 17290240.
- 1 2 Schmahmann, Jeremy D.; Raquel Gardner; Jason MacMore; Mark G. Vangel (2009). "Development of a Brief Ataxia Rating Scale (BARS) based on a modified form of the ICARS". Movement Disorders. 24 (12): 1820–1828. doi:10.1002/mds.22681. PMC 3800087 . PMID 19562773.
- ↑ Weyer, A; et al. (Aug 2007). "Reliability and validity of the scale for the assessment and rating of ataxia: a study in 64 ataxia patients". Movement Disorders. 22 (11): 1633–1637. doi:10.1002/mds.21544. PMID 17516493.