Kwashiorkor is a form of severe protein malnutrition characterized by edema and an enlarged liver with fatty infiltrates. It is thought to be caused by sufficient calorie intake, but with insufficient protein consumption, which distinguishes it from marasmus. Recent studies have found that a lack of antioxidant micronutrients such as β-carotene, lycopene, other carotenoids, and vitamin C as well as the presence of aflatoxins may play a role in the development of the disease. However, the exact cause of kwashiorkor is still unknown. Inadequate food supply is correlated with occurrences of kwashiorkor; occurrences in high income countries are rare. It occurs amongst weaning children to ages of about five years old.
Albuminuria is a pathological condition wherein the protein albumin is abnormally present in the urine. It is a type of proteinuria. Albumin is a major plasma protein ; in healthy people, only trace amounts of it are present in urine, whereas larger amounts occur in the urine of patients with kidney disease. For a number of reasons, clinical terminology is changing to focus on albuminuria more than proteinuria.
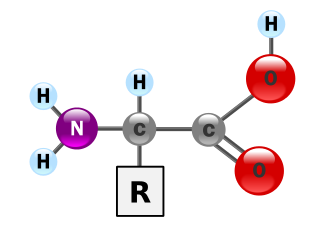
An essential amino acid, or indispensable amino acid, is an amino acid that cannot be synthesized from scratch by the organism fast enough to supply its demand, and must therefore come from the diet. Of the 21 amino acids common to all life forms, the nine amino acids humans cannot synthesize are phenylalanine, valine, threonine, tryptophan, methionine, leucine, isoleucine, lysine, and histidine.

Parenteral nutrition (PN) is the feeding of nutritional products to a person intravenously, bypassing the usual process of eating and digestion. The products are made by pharmaceutical compounding companies. The person receives a nutritional mix according to a formula including glucose, salts, amino acids, lipids and vitamins and dietary minerals. It is called total parenteral nutrition (TPN) or total nutrient admixture (TNA) when no significant nutrition is obtained by other routes, and partial parenteral nutrition (PPN) when nutrition is also partially enteric. It is called peripheral parenteral nutrition (PPN) when administered through vein access in a limb rather than through a central vein as central venous nutrition (CVN).

Cachexia is a complex syndrome associated with an underlying illness causing ongoing muscle loss that is not entirely reversed with nutritional supplementation. A range of diseases can cause cachexia, most commonly cancer, congestive heart failure, chronic obstructive pulmonary disease, chronic kidney disease, and AIDS. Systemic inflammation from these conditions can cause detrimental changes to metabolism and body composition. In contrast to weight loss from inadequate caloric intake, cachexia causes mostly muscle loss instead of fat loss. Diagnosis of cachexia can be difficult due to the lack of well-established diagnostic criteria. Cachexia can improve with treatment of the underlying illness but other treatment approaches have limited benefit. Cachexia is associated with increased mortality and poor quality of life.

Low-carbohydrate diets restrict carbohydrate consumption relative to the average diet. Foods high in carbohydrates are limited, and replaced with foods containing a higher percentage of fat and protein, as well as low carbohydrate foods.
A low-protein diet is a diet in which people decrease their intake of protein. A low-protein diet is used as a therapy for inherited metabolic disorders, such as phenylketonuria and homocystinuria, and can also be used to treat kidney or liver disease. Low protein consumption appears to reduce the risk of bone breakage, presumably through changes in calcium homeostasis. Consequently, there is no uniform definition of what constitutes low-protein, because the amount and composition of protein for an individual with phenylketonuria would differ substantially from one with homocystinuria or tyrosinemia.

Chronic kidney disease (CKD) is a type of kidney disease in which there is gradual loss of kidney function over a period of months to years. Initially there are generally no symptoms; later, symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, and confusion. Complications can relate to hormonal dysfunction of the kidneys and include high blood pressure, bone disease, and anemia. Additionally CKD patients have markedly increased cardiovascular complications with increased risks of death and hospitalization.

Metabolic acidosis is a serious electrolyte disorder characterized by an imbalance in the body's acid-base balance. Metabolic acidosis has three main root causes: increased acid production, loss of bicarbonate, and a reduced ability of the kidneys to excrete excess acids. Metabolic acidosis can lead to acidemia, which is defined as arterial blood pH that is lower than 7.35. Acidemia and acidosis are not mutually exclusive – pH and hydrogen ion concentrations also depend on the coexistence of other acid-base disorders; therefore, pH levels in people with metabolic acidosis can range from low to high.

A high-protein diet is a diet in which 20% or more of the total daily calories comes from protein. Most high protein diets are high in saturated fat and severely restrict intake of carbohydrates.
Protein toxicity is the effect of the buildup of protein metabolic waste compounds, like urea, uric acid, ammonia, and creatinine. Protein toxicity has many causes, including urea cycle disorders, genetic mutations, excessive protein intake, and insufficient kidney function, such as chronic kidney disease and acute kidney injury. Symptoms of protein toxicity include unexplained vomiting and loss of appetite. Untreated protein toxicity can lead to serious complications such as seizures, encephalopathy, further kidney damage, and even death.

In human nutrition, the term empty calories refer to calories found in both beverages and foods composed primarily or solely of sugars and/or certain fats and oils such as cholesterol, saturated or trans fats that provide little to no useful nutrients such as protein, fibre, vitamins, minerals, essential fatty acids, or antioxidants Foods composed mostly of empty calories have low nutrient density, meaning few nutrients relative to their energy content. The consumption of large amounts of empty calories can have negative health consequences.

Protein–energy malnutrition (PEM), sometimes called protein-energy undernutrition (PEU), is a form of malnutrition that is defined as a range of conditions arising from coincident lack of dietary protein and/or energy (calories) in varying proportions. The condition has mild, moderate, and severe degrees.
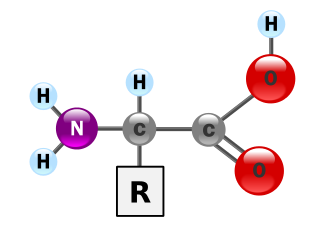
Proteins are essential nutrients for the human body. They are one of the building blocks of body tissue and can also serve as a fuel source. As a fuel, proteins provide as much energy density as carbohydrates: 4 kcal per gram; in contrast, lipids provide 9 kcal per gram. The most important aspect and defining characteristic of protein from a nutritional standpoint is its amino acid composition.
Lactalbumin, also known as "whey protein", is the albumin contained in milk and obtained from whey. Lactalbumin is found in the milk of many mammals. There are alpha and beta lactalbumins; both are contained in milk.
T. Alp Ikizler is a nephrologist, currently holding the Catherine McLaughlin Hakim chair in Medicine at Vanderbilt University School of Medicine, where he does clinical work and heads a research lab. Born in Istanbul, Turkey, he received his M.D. from the Istanbul University Faculty of Medicine.
Specific appetite, also known as specific hunger, is a drive to eat foods with specific flavors or other characteristics.
Calcium acetate/magnesium carbonate is a fixed-dose combination drug that contains 110 mg calcium and 60 mg magnesium ions and is indicated as a phosphate binder for dialysis patients with hyperphosphataemia. It is registered by Fresenius Medical Care under the trade names Renepho (Belgium) and OsvaRen.
Clinical nutrition centers on the prevention, diagnosis, and management of nutritional changes in patients linked to chronic diseases and conditions primarily in health care. Clinical in this sense refers to the management of patients, including not only outpatients at clinics and in private practice, but also inpatients in hospitals. It incorporates primarily the scientific fields of nutrition and dietetics. Furthermore, clinical nutrition aims to maintain a healthy energy balance, while also providing sufficient amounts of nutrients such as protein, vitamins, and minerals to patients.
A renal diet is a diet aimed at keeping levels of fluids, electrolytes, and minerals balanced in the body in individuals with chronic kidney disease or who are on dialysis. Dietary changes may include the restriction of fluid intake, protein, and electrolytes including sodium, phosphorus, and potassium. Calories may also be supplemented if the individual is losing weight undesirably.