Related Research Articles

Carcinoma is a malignancy that develops from epithelial cells. Specifically, a carcinoma is a cancer that begins in a tissue that lines the inner or outer surfaces of the body, and that arises from cells originating in the endodermal, mesodermal or ectodermal germ layer during embryogenesis.

Endometrial cancer is a cancer that arises from the endometrium. It is the result of the abnormal growth of cells that have the ability to invade or spread to other parts of the body. The first sign is most often vaginal bleeding not associated with a menstrual period. Other symptoms include pain with urination, pain during sexual intercourse, or pelvic pain. Endometrial cancer occurs most commonly after menopause.

Ovarian cancer is a cancerous tumor of an ovary. It may originate from the ovary itself or more commonly from communicating nearby structures such as fallopian tubes or the inner lining of the abdomen. The ovary is made up of three different cell types including epithelial cells, germ cells, and stromal cells. When these cells become abnormal, they have the ability to divide and form tumors. These cells can also invade or spread to other parts of the body. When this process begins, there may be no or only vague symptoms. Symptoms become more noticeable as the cancer progresses. These symptoms may include bloating, vaginal bleeding, pelvic pain, abdominal swelling, constipation, and loss of appetite, among others. Common areas to which the cancer may spread include the lining of the abdomen, lymph nodes, lungs, and liver.

Li–Fraumeni syndrome (LFS) is a rare, autosomal dominant, hereditary disorder that predisposes carriers to cancer development. It was named after two American physicians, Frederick Pei Li and Joseph F. Fraumeni Jr., who first recognized the syndrome after reviewing the medical records and death certificates of childhood rhabdomyosarcoma patients. The disease is also known as SBLA, for the Sarcoma, Breast, Leukemia, and Adrenal Gland cancers that it is known to cause.

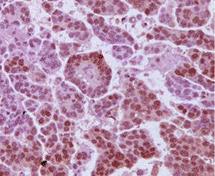
Ovarian clear-cell carcinoma, or clear-cell carcinoma of the ovary, also called ovarian clear-cell adenocarcinoma, is one of several subtypes of ovarian carcinoma – a subtype of epithelial ovarian cancer, in contrast to non-epithelial cancers. According to research, most ovarian cancers start at the epithelial layer which is the lining of the ovary. Within this epithelial group ovarian clear-cell carcinoma makes up 5–10%.

A serous tumour is a neoplasm that typically has papillary to solid formations of tumor cells with crowded nuclei, and which typically arises on the modified Müllerian-derived serous membranes that surround the ovaries in females. Such ovarian tumors are part of the surface epithelial-stromal tumour group of ovarian tumors. They are common neoplasms with a strong tendency to occur bilaterally, and they account for approximately a quarter of all ovarian tumors.

Surface epithelial-stromal tumors are a class of ovarian neoplasms that may be benign or malignant. Neoplasms in this group are thought to be derived from the ovarian surface epithelium or from ectopic endometrial or fallopian tube (tubal) tissue. Tumors of this type are also called ovarian adenocarcinoma. This group of tumors accounts for 90% to 95% of all cases of ovarian cancer; however is mainly only found in postmenopausal women with the exception of the United States where 7% of cases occur in women under the age of 40. Serum CA-125 is often elevated but is only 50% accurate so it is not a useful tumor marker to assess the progress of treatment. 75% of women with epithelial ovarian cancer are found within the advanced-stages; however younger patients are more likely to have better prognoses than older patients.

Personalized medicine, also referred to as precision medicine, is a medical model that separates people into different groups—with medical decisions, practices, interventions and/or products being tailored to the individual patient based on their predicted response or risk of disease. The terms personalized medicine, precision medicine, stratified medicine and P4 medicine are used interchangeably to describe this concept, though some authors and organizations differentiate between these expressions based on particular nuances. P4 is short for "predictive, preventive, personalized and participatory".

Primary peritoneal cancer or carcinoma is also known as serous surface papillary carcinoma, primary peritoneal carcinoma, extra-ovarian serous carcinoma, primary serous papillary carcinoma, and psammomacarcinoma. It was historically classified under "carcinoma of unknown primary" (CUP). Primary peritoneal cancer is a cancer of the cells lining the peritoneum, or abdominal cavity. It usually affects women and is diagnosed after the age of 60; it very rarely affects men.
Gynecologic oncology is a specialized field of medicine that focuses on cancers of the female reproductive system, including ovarian cancer, uterine cancer, vaginal cancer, cervical cancer, and vulvar cancer. As specialists, they have extensive training in the diagnosis and treatment of these cancers.

Primary fallopian tube cancer (PFTC), also known as tubal cancer, is a malignant neoplasm that originates from the fallopian tube. Along with primary ovarian and peritoneal carcinomas, it is grouped under epithelial ovarian cancers; cancers of the ovary that originate from a fallopian tube precursor.

Rucaparib, sold under the brand name Rubraca, is a PARP inhibitor used as an anti-cancer agent. Rucaparib is a first-in-class pharmaceutical drug targeting the DNA repair enzyme poly-ADP ribose polymerase-1 (PARP-1). It is taken by mouth.
A borderline tumor, sometimes called low malignant potential (LMP) tumor, is a distinct but yet heterogeneous group of tumors defined by their histopathology as atypical epithelial proliferation without stromal invasion. It generally refers to such tumors in the ovary but borderline tumors may rarely occur at other locations as well.
A hereditary cancer syndrome is a genetic disorder in which inherited genetic mutations in one or more genes predispose the affected individuals to the development of cancer and may also cause early onset of these cancers. Hereditary cancer syndromes often show not only a high lifetime risk of developing cancer, but also the development of multiple independent primary tumors.
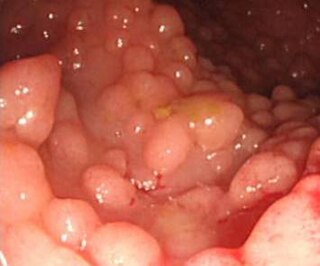
High-grade serous carcinoma (HGSC) is a type of tumour that arises from the serous epithelial layer in the abdominopelvic cavity and is mainly found in the ovary. HGSCs make up the majority of ovarian cancer cases and have the lowest survival rates. HGSC is distinct from low-grade serous carcinoma (LGSC) which arises from ovarian tissue, is less aggressive and is present in stage I ovarian cancer where tumours are localised to the ovary.
Professor Carlos Caldas is a clinician scientist and Professor of Cancer Medicine at the University of Cambridge. He is the Chair of Cancer Medicine at the University of Cambridge, an Honorary Consultant Medical Oncologist at Addenbrooke's Hospital and Director of the Cambridge Breast Cancer Research Unit. He is a fellow of Robinson College, Cambridge and an Emeritus Senior Investigator at the National Institute for Health Research (NIHR).
Serena Nik-Zainal is a British-Malaysian clinician who is a consultant in clinical genetics and Cancer Research UK advanced clinician scientist at the University of Cambridge. She makes use of genomics for clinical applications. She was awarded the Crick Lecture by the Royal Society in 2021. Serena Nik-Zainal was also recognized as one of the 100 Influential Women in Oncology by OncoDaily.
Nitzan Rosenfeld is a professor of Cancer Diagnostics at the University of Cambridge. He is a Senior Group Leader at the Cancer Research UK Cambridge Institute and co-founder of Inivata, a clinical cancer genomics company.

The SEE-FIM protocol is a pathology dissection protocol for Sectioning and Extensively Examining the Fimbria (SEE-FIM). This protocol is intended to provide for the optimal microscopic examination of the distal fallopian tube (fimbria) to identify either cancerous or precancerous conditions in this organ.
Florian Markowetz is the Professor of Computational Oncology at the University of Cambridge. He is a Senior Group Leader at the Cancer Research UK Cambridge Institute and Director and co-founder of Tailor Bio, a genomics company aiming to improve precision medicine for cancers with high levels of chromosomal instability.
References
- ↑ "Dr James Brenton". Cancer Research UK. 2016-07-26. Retrieved 2019-11-18.
- ↑ "Dr James Brenton | Cambridge University Hospitals". www.cuh.nhs.uk. Retrieved 2019-11-18.
- ↑ "Genomics England Announce Lead Researchers". Front Line Genomics. Retrieved 2019-11-18.
- ↑ "New Review of ctDNA Liquid Biopsies in Nature Reviews Cancer Co-Authored by Inivata CSO Nitzan Rosenfeld". Welcome to Inivata. 2017-02-24. Retrieved 2019-11-18.
- ↑ "Dr James Brenton". Cambridge Clinical Informatics. Retrieved 2019-11-18.
- ↑ "Research Gate".
- ↑ Ahmed, Ahmed Ashour; Etemadmoghadam, Dariush; Temple, Jillian; Lynch, Andy G; Riad, Mohamed; Sharma, Raghwa; Stewart, Colin; Fereday, Sian; Caldas, Carlos; deFazio, Anna; Bowtell, David (May 2010). "Driver mutations in TP53 are ubiquitous in high grade serous carcinoma of the ovary". The Journal of Pathology. 221 (1): 49–56. doi:10.1002/path.2696. ISSN 0022-3417. PMC 3262968 . PMID 20229506.
- ↑ Duska, L. R.; Kohn, E. C. (2017-11-01). "The new classifications of ovarian, fallopian tube, and primary peritoneal cancer and their clinical implications". Annals of Oncology. 28 (suppl_8): viii8–viii12. doi:10.1093/annonc/mdx445. ISSN 0923-7534. PMC 6246280 . PMID 29232468.
- ↑ Parkinson, Christine A.; Gale, Davina; Piskorz, Anna M.; Biggs, Heather; Hodgkin, Charlotte; Addley, Helen; Freeman, Sue; Moyle, Penelope; Sala, Evis; Sayal, Karen; Hosking, Karen (2016-12-20). "Exploratory Analysis of TP53 Mutations in Circulating Tumour DNA as Biomarkers of Treatment Response for Patients with Relapsed High-Grade Serous Ovarian Carcinoma: A Retrospective Study". PLOS Medicine. 13 (12): e1002198. doi: 10.1371/journal.pmed.1002198 . ISSN 1549-1676. PMC 5172526 . PMID 27997533.
- ↑ "Searching for a blood test to monitor ovarian cancer". Cancer Research UK - Science blog. 20 December 2016. Retrieved 2019-11-18.
- ↑ Schwarz, Roland F.; Ng, Charlotte K. Y.; Cooke, Susanna L.; Newman, Scott; Temple, Jillian; Piskorz, Anna M.; Gale, Davina; Sayal, Karen; Murtaza, Muhammed; Baldwin, Peter J.; Rosenfeld, Nitzan (2015-02-24). "Spatial and Temporal Heterogeneity in High-Grade Serous Ovarian Cancer: A Phylogenetic Analysis". PLOS Medicine. 12 (2): e1001789. doi: 10.1371/journal.pmed.1001789 . ISSN 1549-1676. PMC 4339382 . PMID 25710373.
- ↑ "'Patchwork' ovarian cancer more deadly". Cancer Research UK. 2015-02-24. Retrieved 2019-11-18.
- ↑ "Ovarian cancer more deadly if in 'patchwork' pattern | Cambridge University Hospitals". www.cuh.nhs.uk. Retrieved 2019-11-18.
- ↑ "Unpicking the genetic 'patchwork' in ovarian cancer". Cancer Research UK - Science blog. Retrieved 2019-11-18.
- ↑ "'Patchwork' ovarian cancer is most deadly". The Best Of Health. 4 March 2015. Retrieved 2019-11-18.
- ↑ Macintyre, Geoff; Goranova, Teodora E.; De Silva, Dilrini; Ennis, Darren; Piskorz, Anna M.; Eldridge, Matthew; Sie, Daoud; Lewsley, Liz-Anne; Hanif, Aishah; Wilson, Cheryl; Dowson, Suzanne (September 2018). "Copy number signatures and mutational processes in ovarian carcinoma". Nature Genetics. 50 (9): 1262–1270. doi:10.1038/s41588-018-0179-8. ISSN 1546-1718. PMC 6130818 . PMID 30104763.
- ↑ "Unravelling ovarian cancer genome complexity – NIHR Imperial Biomedical Research Centre" . Retrieved 2019-11-18.
- ↑ "Ovarian cancer genetics unravelled | Imperial News | Imperial College London" . Retrieved 2019-11-18.
- ↑ "Exciting new research could lead to personalised ovarian cancer treatments". Ovarian Cancer Action. Retrieved 2019-11-18.
- ↑ "BriTROC-2". Ovarian cancer Action. Retrieved 2019-11-18.