Related Research Articles

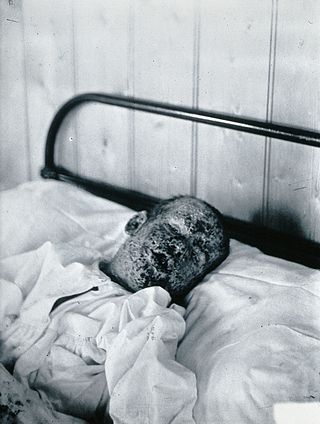
Rubella, also known as German measles or three-day measles, is an infection caused by the rubella virus. This disease is often mild, with half of people not realizing that they are infected. A rash may start around two weeks after exposure and last for three days. It usually starts on the face and spreads to the rest of the body. The rash is sometimes itchy and is not as bright as that of measles. Swollen lymph nodes are common and may last a few weeks. A fever, sore throat, and fatigue may also occur. Joint pain is common in adults. Complications may include bleeding problems, testicular swelling, encephalitis, and inflammation of nerves. Infection during early pregnancy may result in a miscarriage or a child born with congenital rubella syndrome (CRS). Symptoms of CRS manifest as problems with the eyes such as cataracts, deafness, as well as affecting the heart and brain. Problems are rare after the 20th week of pregnancy.

The Pan American Health Organization (PAHO) is a specialized agency of the United Nations (UN) in charge of international health cooperation in the Americas. It fosters technical cooperation among member countries to fight communicable and noncommunicable diseases, strengthen health systems, and respond to emergencies and disasters. It has 35 Member States and four Associate Members in the region. Headquartered in Washington, D.C., PAHO is the regional office for the World Health Organization in the Americas, and the health organization of the Inter-American System. It is known in Latin America as the OPS or OPAS.

Polio eradication, the permanent global cessation of circulation of the poliovirus and hence elimination of the poliomyelitis (polio) it causes, is the aim of a multinational public health effort begun in 1988, led by the World Health Organization (WHO), the United Nations Children's Fund (UNICEF) and the Rotary Foundation. These organizations, along with the U.S. Centers for Disease Control and Prevention (CDC) and The Gates Foundation, have spearheaded the campaign through the Global Polio Eradication Initiative (GPEI). Successful eradication of infectious diseases has been achieved twice before, with smallpox in humans and rinderpest in ruminants.
Operation MECACAR is a multi-national immunization program launched in 1995 by the World Health Organization to coordinate polio vaccination efforts. The name of the operation was derived from the names of the regions participating in the operation: Eastern Mediterranean, Caucasus, Central Asian Republics and Russia. Currently, 18 countries are participating and more than 60 million children have been vaccinated.

Ciro Carlos Araujo de Quadros was a Brazilian leader in the field of Public Health, in particular, the area of vaccines and preventable diseases. He was born in Rio Pardo, Brazil.
The eradication of infectious diseases is the reduction of the prevalence of an infectious disease in the global host population to zero.
The Expanded Program on Immunization is a World Health Organization program with the goal to make vaccines available to all children.

Mirta Roses Periago is an Argentine epidemiologist who served as Director of the Pan American Health Organization (PAHO) from 2003 until 2013.
Jean Marie Okwo-Bele is a Congolese physician, public health expert and former Director of the Department of Immunization, Vaccines and Biologicals of the World Health Organization (WHO).

Measles vaccine protects against becoming infected with measles. Nearly all of those who do not develop immunity after a single dose develop it after a second dose. When the rate of vaccination within a population is greater than 92%, outbreaks of measles typically no longer occur; however, they may occur again if the rate of vaccination decreases. The vaccine's effectiveness lasts many years. It is unclear if it becomes less effective over time. The vaccine may also protect against measles if given within a couple of days after exposure to measles.

Rubella vaccine is a vaccine used to prevent rubella. Effectiveness begins about two weeks after a single dose and around 95% of people become immune. Countries with high rates of immunization no longer see cases of rubella or congenital rubella syndrome. When there is a low level of childhood immunization in a population it is possible for rates of congenital rubella to increase as more women make it to child-bearing age without either vaccination or exposure to the disease. Therefore, it is important for more than 80% of people to be vaccinated. By introducing rubella containing vaccines, rubella has been eradicated in 81 nations, as of mid-2020.
Universal Immunisation Programme (UIP) is a vaccination programme launched by the Government of India in 1985. It became a part of Child Survival and Safe Motherhood Programme in 1992 and is currently one of the key areas under the National Health Mission since 2005. The programme now consists of vaccination for 12 diseases- tuberculosis, diphtheria, pertussis, tetanus, poliomyelitis, measles, hepatitis B, rotaviral gastroenteritis, Japanese encephalitis, rubella, pneumonia and Pneumococcal diseases. Hepatitis B and Pneumococcal diseases were added to the UIP in 2007 and 2017 respectively. The cost of all the vaccines are borne entirely by the Government of India and is funded through taxes with a budget of ₹7,234 crore (US$910 million) in 2022 and the program covers all residents of India, including foreign residents.
India National PolioPlus Society is a non-profit organization. The Initiative has achieved significant progress toward its goals. There has been a dramatic decline in cases everywhere in the seventeen years since the target was set in 1988.

The Global Polio Eradication Initiative is an initiative created in 1988, just after the World Health Assembly resolved to eradicate the disease poliomyelitis. Led by the World Health Organization, it is the largest international public health initiative in history.
Isao Arita was a Japanese physician, virologist and vaccination specialist who headed the World Health Organization (WHO) Smallpox Eradication Unit in 1977–85. During this period, smallpox became the first infectious disease of humans to be eradicated globally. For this work, he and his colleagues were awarded the Japan Prize in 1988. He also advised the successful programme to eradicate poliovirus from the Western Pacific region.
Dr. Robert Kezaala is a medical doctor, epidemiologist, scholar and public health leader in the field of immunization and health emergencies. Currently he is serving as a Senior Health Advisor and team lead for Accelerated Immunization Initiatives: measles, rubella, epidemic meningitis and yellow fever control and Immunization in Emergencies at the United Nations Children’s Fund.

Michael Joseph Ryan is an Irish epidemiologist and former trauma surgeon, specialising in infectious disease and public health. He is executive director of the World Health Organization's Health Emergencies Programme, leading the team responsible for the international containment and treatment of COVID-19. Ryan has held leadership positions and has worked on various outbreak response teams in the field to eradicate the spread of diseases including bacillary dysentery, cholera, Crimean–Congo hemorrhagic fever, Ebola, Marburg virus disease, measles, meningitis, relapsing fever, Rift Valley fever, SARS, and Shigellosis.
The World Health Organization (WHO) created the Global Commission for the Certification of the Eradication of Poliomyelitis in 1995 to independently verify the eradication of wild poliovirus. The GCC certified the worldwide eradication of indigenous wild poliovirus type 2 on 20 September 2015, and wild poliovirus type 3 on 17 October 2019. In addition, five of the six World Health Organization Regions certified their status as free of indigenous transmission of all three serotypes of wild poliovirus :
The Strategic Advisory Group of Experts (SAGE) is the principal advisory group to World Health Organization (WHO) for vaccines and immunization. Established in 1999 through the merging of two previous committees, notably the Scientific Advisory Group of Experts and the Global Advisory Group by Director-General of the WHO Gro Harlem Brundtland. It is charged with advising WHO on overall global policies and strategies, ranging from vaccines and biotechnology, research and development, to delivery of immunization and its linkages with other health interventions. SAGE is concerned not just with childhood vaccines and immunization, but all vaccine-preventable diseases. SAGE provide global recommendations on immunization policy and such recommendations will be further translated by advisory committee at the country level.
Folake Olayinka, physician and global health leader. Since October 2020, she has served as the United States Agency for International Development's (USAID) Global Immunization lead/STAR Fellow. She also served as Technical and Strategy lead for the COVID19 Vaccine Access and Delivery Initiative Washington DC, United States.
References
- ↑ Aylward Bruce, Andrus Jon, Bilous Julian, Smith Jean, Sanders Ray (1997). "Pollomyelitis immunisation programmes". The Lancet. 349 (9051): 574–575. doi: 10.1016/S0140-6736(97)80127-4 . PMID 9048817. S2CID 54288033.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ PAHO. "Dr. Jon Andrus is Named PAHO Deputy Director" . Retrieved 27 November 2013.
- ↑ World Vaccine Congress. "Dr Jon K. Andrus, Deputy Director". Archived from the original on 2 December 2013. Retrieved 27 November 2013.
- ↑ "Research | Colorado School of Public Health".
- ↑ "OPAS/OMS | Dr. Jon Andrus is Named PAHO Deputy Director". 28 September 2009.
- ↑ Andrus JK, Thapa AB, Withana N, Fitzsimmons JW, Abeykoon P, Aylward B (2001). "A new paradigm for international disease control: lessons learned from polio eradication in Southeast Asia". Am J Public Health. 91 (1): 146–50. doi:10.2105/ajph.91.1.146. PMC 1446512 . PMID 11189812.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ "Jon Kim Andrus publications" . Retrieved 27 November 2013.
- ↑ Zimmerman, Rick S.; Diclemente, Ralph J.; Andrus, Jon K.; Hosein, Everold N. (2016-05-16). Introduction to Global Health Promotion. John Wiley & Sons. ISBN 9781118897799.
- ↑ worldcongress.com. "Speaker Biography". Archived from the original on 3 December 2013. Retrieved 27 November 2013.
- ↑ "UCSF researcher receives distinguished service medal for his work in eradicating polio in southeast asia". www.eurekalert.org. Archived from the original on 2002-03-21.
- ↑ "GPEI-Global Polio Partners Group".
- ↑ Polio Transition Independent Monitoring Board (TIMB) Archived 2016-11-09 at the Wayback Machine Global Polio Eradication Initiative (GPEI)
- ↑ "OPAS/OMS | Reports of the Technical Advisory Group (TAG) on Vaccine-preventable Diseases". 2 October 2009.
- ↑ "World Health Organization, Third Meeting of the South East Asia Regional Verification Commission on Measles Rubella and Congenital Rubella Syndrome (SEA-RVC)". www.searo.who.int. Archived from the original on 2 November 2018. Retrieved 17 January 2022.