Related Research Articles
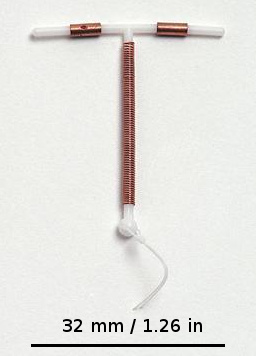
A copper intrauterine device (IUD), also known as an intrauterine coil or copper coil or non-hormonal IUD, is a type of intrauterine device which contains copper. It is used for birth control and emergency contraception within five days of unprotected sex. It is one of the most effective forms of birth control with a one-year failure rate around 0.7%. The device is placed in the uterus and lasts up to twelve years. It may be used by women of all ages regardless of whether or not they have had children. Following removal, fertility quickly returns.

Emergency contraception (EC) is a birth control measure, used after sexual intercourse to prevent pregnancy.

Family planning is the consideration of the number of children a person wishes to have, including the choice to have no children, and the age at which they wish to have them. Things that may play a role on family planning decisions include marital situation, career or work considerations, financial situations. If sexually active, family planning may involve the use of contraception and other techniques to control the timing of reproduction.
The Planned Parenthood Federation of America, Inc. (PPFA), or simply Planned Parenthood, is a 501(c)(3) nonprofit organization that provides reproductive and sexual healthcare, and sexual education in the United States and globally. It is a member of the International Planned Parenthood Federation (IPPF).

A hormonal intrauterine device (IUD), also known as an intrauterine system (IUS) with progestogen and sold under the brand name Mirena among others, is an intrauterine device that releases a progestogenic hormonal agent such as levonorgestrel into the uterus. It is used for birth control, heavy menstrual periods, and to prevent excessive build of the lining of the uterus in those on estrogen replacement therapy. It is one of the most effective forms of birth control with a one-year failure rate around 0.2%. The device is placed in the uterus and lasts three to eight years. Fertility often returns quickly following removal.

Hormonal contraception refers to birth control methods that act on the endocrine system. Almost all methods are composed of steroid hormones, although in India one selective estrogen receptor modulator is marketed as a contraceptive. The original hormonal method—the combined oral contraceptive pill—was first marketed as a contraceptive in 1960. In the ensuing decades, many other delivery methods have been developed, although the oral and injectable methods are by far the most popular. Hormonal contraception is highly effective: when taken on the prescribed schedule, users of steroid hormone methods experience pregnancy rates of less than 1% per year. Perfect-use pregnancy rates for most hormonal contraceptives are usually around the 0.3% rate or less. Currently available methods can only be used by women; the development of a male hormonal contraceptive is an active research area.
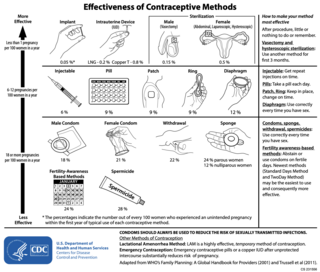
There are many methods of birth control that vary in requirements, side effects, and effectiveness. As the technology, education, and awareness about contraception has evolved, new contraception methods have been theorized and put in application. Although no method of birth control is ideal for every user, some methods remain more effective, affordable or intrusive than others. Outlined here are the different types of barrier methods, hormonal methods, various methods including spermicides, emergency contraceptives, and surgical methods and a comparison between them.
Long-acting reversible contraceptives (LARC) are methods of birth control that provide effective contraception for an extended period without requiring user action. They include hormonal and non-hormonal intrauterine devices (IUDs), and subdermal hormonal contraceptive implants. They are the most effective reversible methods of contraception because their efficacy is not reliant on patient compliance. The failure rates of IUDs and implants is less than 1% per year.

A contraceptive implant is an implantable medical device used for the purpose of birth control. The implant may depend on the timed release of hormones to hinder ovulation or sperm development, the ability of copper to act as a natural spermicide within the uterus, or it may work using a non-hormonal, physical blocking mechanism. As with other contraceptives, a contraceptive implant is designed to prevent pregnancy, but it does not protect against sexually transmitted infections.

Birth control, also known as contraception, anticonception, and fertility control, is the use of methods or devices to prevent unintended pregnancy. Birth control has been used since ancient times, but effective and safe methods of birth control only became available in the 20th century. Planning, making available, and using human birth control is called family planning. Some cultures limit or discourage access to birth control because they consider it to be morally, religiously, or politically undesirable.
The Family Planning Services and Population Research Act of 1970 is the only federal grant program dedicated to providing individuals with comprehensive family planning and related preventive health services. It was signed into law under President Richard Nixon on December 24, 1970.
Unintended pregnancies are pregnancies that are mistimed or unwanted at the time of conception, also known as unplanned pregnancies.
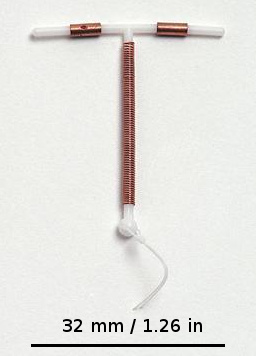
An intrauterine device (IUD), also known as intrauterine contraceptive device or coil, is a small, often T-shaped birth control device that is inserted into the uterus to prevent pregnancy. IUDs are one form of long-acting reversible birth control (LARC). One study found that female family planning providers choose LARC methods more often (41.7%) than the general public (12.1%). Among birth control methods, IUDs, along with other contraceptive implants, result in the greatest satisfaction among users.

The Responsible Parenthood and Reproductive Health Act of 2012, also known as the Reproductive Health Law or RH Law, and officially designated as Republic Act No. 10354, is a Philippine law that provided universal access to methods on contraception, fertility control, sexual education, and maternal care.

Birth control in the United States is available in many forms. Some of the forms available at drugstores and some retail stores are male condoms, female condoms, sponges, spermicides, and over-the-counter emergency contraception. Forms available at pharmacies with a doctor's prescription or at doctor's offices are oral contraceptive pills, patches, vaginal rings, diaphragms, shots/injections, cervical caps, implantable rods, and intrauterine devices (IUDs). Sterilization procedures, including tubal ligations and vasectomies, are also performed.
A contraceptive mandate is a government regulation or law that requires health insurers, or employers that provide their employees with health insurance, to cover some contraceptive costs in their health insurance plans.
The objective of family planning in the United States is to enable individuals to determine the number and spacing of their children and to select the means by which that target may be achieved. Doing so can bring many benefits including improved maternal health, the prevention of the spread of STDs, and decreased infant and child mortality rates.
Women's reproductive health in the United States refers to the set of physical, mental, and social issues related to the health of women in the United States. It includes the rights of women in the United States to adequate sexual health, available contraception methods, and treatment for sexually transmitted diseases. The prevalence of women's health issues in American culture is inspired by second-wave feminism in the United States. As a result of this movement, women of the United States began to question the largely male-dominated health care system and demanded a right to information on issues regarding their physiology and anatomy. The U.S. government has made significant strides to propose solutions, like creating the Women's Health Initiative through the Office of Research on Women's Health in 1991. However, many issues still exist related to the accessibility of reproductive healthcare as well as the stigma and controversy attached to sexual health, contraception, and sexually transmitted diseases.
The Texas Policy Evaluation Project, or TxPEP, is a collaborative group of university-based investigators who evaluate the impact of legislation in Texas related to women's reproductive health. It began in the fall of 2011 with the purpose of documenting and evaluating the impact of reproductive health legislation passed by the 82nd Texas Legislature. Those measures included large cuts to state family planning funding programs in the 2012–2013 budget as well as changes in the eligibility of organizations to participate in those programs, and Texas House Bill 15, a law requiring that women undergo a mandatory sonogram at least 24 hours before an abortion.

Maternal healthcare in Texas refers to the provision of family planning services, abortion options, pregnancy-related services, and physical and mental well-being care for women during the prenatal and postpartum periods. The provision of maternal health services in each state can prevent and reduce the incidence of maternal morbidity and mortality and fetal death.
References
- ↑ "Joseph Potter". UT College of Liberal Arts. Retrieved 2017-09-15.
- ↑ "Joseph Potter". Demographic Research. Retrieved 2017-09-15.
- ↑ "Study: Texas birth control fell after Planned Parenthood cut". CBS News. 2016-02-03. Retrieved 2017-09-15.
- ↑ Zernike, Kate (2017-03-14). "Cutting Planned Parenthood Would Increase Medicaid Births, C.B.O. Says". The New York Times. ISSN 0362-4331 . Retrieved 2017-09-15.
- ↑ Flynn, Meagan (2017-07-17). "Despite Demand, Few Texas Women on Medicaid Are Able to Access IUDs". Houston Press. Retrieved 2017-09-15.
- ↑ "It is with heavy hearts that we share the loss of our colleague and Professor Emeritus Joe Potter". University of Texas at Austin. May 14, 2024. Retrieved May 21, 2024.
- ↑ Nota de Pesar – Professor Doutor Joseph E. Potter (in Portuguese)