Related Research Articles

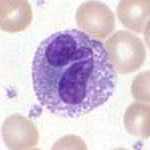
Macrophages are a type of white blood cell of the innate immune system that engulf and digest pathogens, such as cancer cells, microbes, cellular debris, and foreign substances, which do not have proteins that are specific to healthy body cells on their surface. This process is called phagocytosis, which acts to defend the host against infection and injury.

Neutrophils are the most abundant type of granulocytes and make up 40% to 70% of all white blood cells in humans. They form an essential part of the innate immune system, with their functions varying in different animals.

Phagocytes are cells that protect the body by ingesting harmful foreign particles, bacteria, and dead or dying cells. Their name comes from the Greek phagein, "to eat" or "devour", and "-cyte", the suffix in biology denoting "cell", from the Greek kutos, "hollow vessel". They are essential for fighting infections and for subsequent immunity. Phagocytes are important throughout the animal kingdom and are highly developed within vertebrates. One litre of human blood contains about six billion phagocytes. They were discovered in 1882 by Ilya Ilyich Mechnikov while he was studying starfish larvae. Mechnikov was awarded the 1908 Nobel Prize in Physiology or Medicine for his discovery. Phagocytes occur in many species; some amoebae behave like macrophage phagocytes, which suggests that phagocytes appeared early in the evolution of life.

Monocytes are a type of leukocyte or white blood cell. They are the largest type of leukocyte in blood and can differentiate into macrophages and monocyte derived dendritic cells. As a part of the vertebrate innate immune system monocytes also influence adaptive immune responses and exert tissue repair functions. There are at least three subclasses of monocytes in human blood based on their phenotypic receptors.
Granulocytes are cells in the innate immune system characterized by the presence of specific granules in their cytoplasm. Such granules distinguish them from the various agranulocytes. All myeloblastic granulocytes are polymorphonuclear. They have varying shapes (morphology) of the nucleus ; and are referred to as polymorphonuclear leukocytes. In common terms, polymorphonuclear granulocyte refers specifically to "neutrophil granulocytes", the most abundant of the granulocytes; the other types have varying morphology. Granulocytes are produced via granulopoiesis in the bone marrow.

Chemokines, or chemotactic cytokines, are a family of small cytokines or signaling proteins secreted by cells that induce directional movement of leukocytes, as well as other cell types, including endothelial and epithelial cells. In addition to playing a major role in the activation of host immune responses, chemokines are important for biological processes, including morphogenesis and wound healing, as well as in the pathogenesis of diseases like cancers.
A histiocyte is a vertebrate cell that is part of the mononuclear phagocyte system. The mononuclear phagocytic system is part of the organism's immune system. The histiocyte is a tissue macrophage or a dendritic cell. Part of their job is to clear out neutrophils once they've reached the end of their lifespan.

The innate, or nonspecific, immune system is one of the two main immunity strategies in vertebrates. The innate immune system is an alternate defense strategy and is the dominant immune system response found in plants, fungi, insects, and primitive multicellular organisms.

CD11c, also known as Integrin, alpha X (ITGAX), is a gene that encodes for CD11c.

Integrin alpha M (ITGAM) is one protein subunit that forms heterodimeric integrin alpha-M beta-2 (αMβ2) molecule, also known as macrophage-1 antigen (Mac-1) or complement receptor 3 (CR3). ITGAM is also known as CR3A, and cluster of differentiation molecule 11B (CD11B). The second chain of αMβ2 is the common integrin β2 subunit known as CD18, and integrin αMβ2 thus belongs to the β2 subfamily integrins.
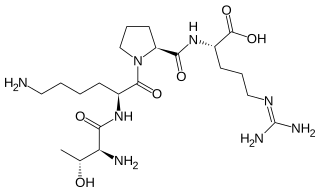
Tuftsin is a tetrapeptide located in the Fc-domain of the heavy chain of immunoglobulin G. It has an immunostimulatory effect. It is named for Tufts University where it was first discovered in 1983.
In anatomy and histology, the term wandering cell is used to describe cells that are found in connective tissue, but are not fixed in place. This term is used occasionally and usually refers to blood leukocytes in particular mononuclear phagocytes. Frequently, the term refers to circulating macrophages and has been used also for stationary macrophages fixed in tissues (histiocytes), which are sometimes referred to as "resting wandering cells".

Integrin α4β1 is an integrin dimer. It is composed of CD49d and CD29. The alpha 4 subunit is 155 kDa, and the beta 1 subunit is 150 kDa.
CD16, also known as FcγRIII, is a cluster of differentiation molecule found on the surface of natural killer cells, neutrophils, monocytes, macrophages, and certain T cells. CD16 has been identified as Fc receptors FcγRIIIa (CD16a) and FcγRIIIb (CD16b), which participate in signal transduction. The most well-researched membrane receptor implicated in triggering lysis by NK cells, CD16 is a molecule of the immunoglobulin superfamily (IgSF) involved in antibody-dependent cellular cytotoxicity (ADCC). It can be used to isolate populations of specific immune cells through fluorescent-activated cell sorting (FACS) or magnetic-activated cell sorting, using antibodies directed towards CD16.
A non-specific immune cell is an immune cell that responds to many antigens, not just one antigen. Non-specific immune cells function in the first line of defense against infection or injury. The innate immune system is always present at the site of infection and ready to fight the bacteria; it can also be referred to as the "natural" immune system. The cells of the innate immune system do not have specific responses and respond to each foreign invader using the same mechanism.

White blood cells, also called leukocytes or leucocytes, are cells of the immune system that are involved in protecting the body against both infectious disease and foreign invaders. White blood cells include three main subtypes; granulocytes, lymphocytes and monocytes.
The pluripotency of biological compounds describes the ability of certain substances to produce several distinct biological responses. Pluripotent is also described as something that has no fixed developmental potential, as in being able to differentiate into different cell types in the case of pluripotent stem cells.
Intravascular immunity describes the immune response in the bloodstream, and its role is to fight and prevent the spread of pathogens. Components of intravascular immunity include the cellular immune response and the macromolecules secreted by these cells. It can result in responses such as inflammation and immunothrombosis. Dysregulated intravascular immune response or pathogen evasion can create conditions like thrombosis, sepsis, or disseminated intravascular coagulation.

Toxic vacuolation, also known as toxic vacuolization, is the formation of vacuoles in the cytoplasm of neutrophils in response to severe infections or inflammatory conditions.

Artificial white blood cells are typically membrane bound vesicles designed to mimic the immunomodulatory behavior of naturally produced leukocytes. While extensive research has been done with regards to artificial red blood cells and platelets for use in emergency blood transfusions, research into artificial white blood cells has been focused on increasing the immunogenic response within a host to treat cancer or deliver drugs in a more favorable fashion. While certain limitations have prevented leukocyte mimicking particles from becoming widely used and FDA approved, more research is being allocated to this area of synthetic blood which has the potential for producing a new form of treatment for cancer and other diseases.
References
- ↑ Ghai CL (2013). A textbook of practical physiology (8th ed.). New Delhi: Jaypee Bros. Medical Publishers. p. 65. ISBN 9789350259320.