Related Research Articles

Haemophilia or hemophilia, is a mostly inherited genetic disorder that impairs the body's ability to make blood clots, a process needed to stop bleeding. This results in people bleeding for a longer time after an injury, easy bruising, and an increased risk of bleeding inside joints or the brain. Those with a mild case of the disease may have symptoms only after an accident or during surgery. Bleeding into a joint can result in permanent damage while bleeding in the brain can result in long term headaches, seizures, or a decreased level of consciousness.

Haemophilia A is a genetic deficiency in clotting factor VIII, which causes increased bleeding and usually affects males. In the majority of cases it is inherited as an X-linked recessive trait, though there are cases which arise from spontaneous mutations.

A blood-borne disease is a disease that can be spread through contamination by blood and other body fluids. Blood can contain pathogens of various types, chief among which are microorganisms, like bacteria and parasites, and non-living infectious agents such as viruses. Three bloodborne pathogens in particular, all viruses, are cited as of primary concern to health workers by the CDC-NIOSH: HIV, hepatitis B (HVB), & hepatitis C (HVC).
The Japanese HIV-tainted blood scandal, refers to an event in the 1980s when between one and two thousand haemophilia patients in Japan contracted HIV via tainted blood products. Controversy centered on the continued use of non-heat-treated blood products after the development of heat treatments that prevented the spread of infection. Some high-ranking officials in the Ministry of Health and Welfare, executives of the manufacturing company and a leading doctor in the field of haemophilia study were charged for involuntary manslaughter.

The tainted blood disaster, or the tainted blood scandal, was a Canadian public health crisis in the 1980s in which thousands of people were exposed to HIV and hepatitis C through contaminated blood products. It became apparent that inadequately-screened blood, often coming from high-risk populations, was entering the system through blood transfusions. It is now considered to be the largest single (preventable) public health disaster in the history of Canada.

In England, blood and other tissues are collected by NHS Blood and Transplant (NHSBT). NHSBT Blood Donation was previously known as the National Blood Service until it merged with UK Transplant in 2005 to form a NHS special health authority. Other official blood services in the United Kingdom include the Northern Ireland Blood Transfusion Service, the Scottish National Blood Transfusion Service and the Welsh Blood Service.
The Irish Blood Transfusion Service (IBTS), or Seirbhís Fuilaistriúcháin na hÉireann in Irish, was established in Ireland as the Blood Transfusion Service Board (BTSB) by the Blood Transfusion Service Board (Establishment) Order, 1965. It took its current name in April 2000 by Statutory Instrument issued by the Minister for Health and Children to whom it is responsible. The Service provides blood and blood products for humans.

Factor 8: The Arkansas Prison Blood Scandal is a feature-length documentary by Arkansas filmmaker and investigative journalist Kelly Duda. Through interviews and presentation of documents and footage, Duda alleges that for more than two decades, spanning the 1970s and 1980s, the Arkansas prison system profited from selling blood plasma from inmates infected with viral hepatitis and HIV. The documentary contends that thousands of victims who received transfusions of a blood product derived from these plasma products, Factor VIII, died as a result.
Contaminated haemophilia blood products were a serious public health problem in the late 1970s up to 1985.
France's infected blood scandal began in April 1991 when doctor and journalist Anne-Marie Casteret published an article in the weekly magazine the L'Événement du jeudi proving that the Centre National de Transfusion Sanguine knowingly distributed blood products contaminated with HIV to haemophiliacs in 1984 and 1985, causing a multi-national outbreak of HIV and hepatitis C. It is estimated that 6000 to 10000 haemophiliacs were infected in the United States alone. In France 4700 people were contaminated, over 300 died. Other impacted countries include Canada, Iran, Iraq, Ireland, Italy, Japan, Portugal, and the United Kingdom.
A transfusion transmitted infection (TTI) is a virus, parasite, or other potential pathogen that can be transmitted in donated blood through a transfusion to a recipient. The term is usually limited to known pathogens, but also sometimes includes agents such as Simian foamy virus which are not known to cause disease.
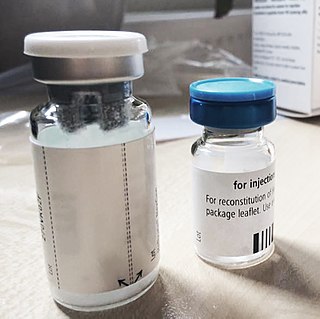
The contaminated blood scandal in the United Kingdom arose when at least 3,891 people, most of whom suffered from haemophilia, became infected with hepatitis C of whom 1,243 were also infected with HIV, the virus that leads to acquired immune deficiency syndrome (AIDS), as a result of receiving contaminated clotting factor products supplied by the National Health Service (NHS) in the 1970s and 1980s. As of October 2017 there were at least 1,246 confirmed deaths in the UK of people who were killed by the use of contaminated factor VIII and factor IX clotting agents and the viruses they transmitted. Some have estimated that the total number of those who have died could be as high as 2,400 though exact figures are not known.

Jeanne Marie Lusher, M.D. was an American physician, pediatric hematologist/oncologist, and a researcher in the field of bleeding disorders of childhood, and has served as the director of Hemostasis Program at the Children's Hospital of Michigan until her retirement on June 28, 2013.

David Maurice Surrey Dane, MRCS CRCP MB Bchir MRCP MRCPath FRCPath FRCP was a pre-eminent British pathologist and clinical virologist known for his pioneering work in infectious diseases including poliomyelitis and the early investigations into the efficacy of a number of vaccines. He is particularly remembered for his strategic foresight in the field of blood transfusion microbiology, particularly in relation to diseases that are spread through blood transfusion.
The Penrose Inquiry was the public inquiry into hepatitis C and HIV infections from NHS Scotland treatment with blood and blood products such as factor VIII, often used by people with haemophilia. The event is often called the Tainted Blood Scandal or Contaminated Blood Scandal.

A and Others v National Blood Authority and Another, also known as the Hepatitis C Litigation, was a landmark product liability case of 2001 primarily concerning blood transfusions but also blood products or transplanted organs, all of which were infected with hepatitis C, where liability was established under the Consumer Protection Act 1987 and the Product Liability Directive (85/374/EEC) even in the absence of the ability to test to ascertain which blood transfusions were defective. The claimants were 114 individuals, six of whom were considered lead plaintiffs and given close consideration by the judge, Mr Justice Burton. Several of the claimants were minors who had become infected with Hepatitis C in the course of their treatment for leukaemia. The defendants were the National Blood Authority (NBA) and in respect of Wales, the Velindre NHS Trust, Cardiff. The court found that the UK government should have implemented measures to screen donated blood for HCV by March 1990, rather than September 1991.
Brigid McCole was an Irish hepatitis C campaigner.

The HIV Haemophilia Litigation [1990] 41 BMLR 171, [1990] 140 NLJR 1349 (CA), [1989] E N. 2111, also known as AMcG002, and HHL, was a legal claim by 962 plaintiffs, mainly haemophiliacs, who were infected with HIV as a result of having been treated with blood products in the late 1970s and early 1980s. The first central defendants were the then Department of Health, with other defendants being the Licensing Authority of the time, (MCA), the CSM, the CBLA, and the regional health authorities of England and Wales.
In 1994, the Irish Blood Transfusion Service Board (BTSB) informed the Minister for Health that a blood product they had distributed in 1977 for the treatment of pregnant mothers had been contaminated with the Hepatitis C virus. Following a report by an expert group, it was discovered that the BTSB had produced and distributed a second infected batch in 1991. The Government established a Tribunal of Enquiry to establish the facts of the case and also agreed to establish a tribunal for the compensation of victims but seemed to frustrate and delay the applications of these, in some cases terminally, ill women.
The Irish Haemophilia Society (IHS) is an organization that represents the interests of people with haemophilia, von Willebrand’s disease and other inherited bleeding disorders.
References
- "Report of the Tribunal of Inquiry into the Infection with HIV and Hepatitis C of Persons with Haemophilia and Related Matters". Department of Health. 5 September 2002. Retrieved 16 September 2014.