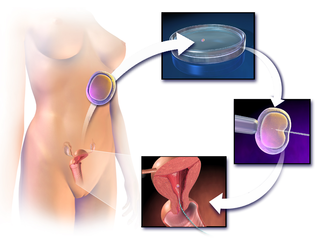
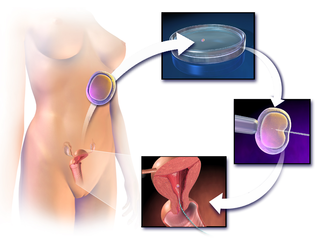
In vitro fertilisation (IVF) is a process of fertilisation where an egg is combined with sperm in vitro. The process involves monitoring and stimulating a patient's ovulatory process, removing an ovum or ova from their ovaries and letting sperm fertilise them in a culture medium in a laboratory. After the fertilised egg (zygote) undergoes embryo culture for 2–6 days, it is transferred by catheter into the uterus, with the intention of establishing a successful pregnancy.

The Human Fertilisation and Embryology Authority (HFEA) is an executive non-departmental public body of the Department of Health and Social Care in the United Kingdom. It is a statutory body that regulates and inspects all clinics in the United Kingdom providing in vitro fertilisation (IVF), artificial insemination and the storage of human eggs, sperm or embryos. It also regulates human embryo research.
Assisted reproductive technology (ART) includes medical procedures used primarily to address infertility. This subject involves procedures such as in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), cryopreservation of gametes or embryos, and/or the use of fertility medication. When used to address infertility, ART may also be referred to as fertility treatment. ART mainly belongs to the field of reproductive endocrinology and infertility. Some forms of ART may be used with regard to fertile couples for genetic purpose. ART may also be used in surrogacy arrangements, although not all surrogacy arrangements involve ART. The existence of sterility will not always require ART to be the first option to consider, as there are occasions when its cause is a mild disorder that can be solved with more conventional treatments or with behaviors based on promoting health and reproductive habits.

A sperm bank, semen bank, or cryobank is a facility or enterprise which purchases, stores and sells human semen. The semen is produced and sold by men who are known as sperm donors. The sperm is purchased by or for other persons for the purpose of achieving a pregnancy or pregnancies other than by a sexual partner. Sperm sold by a sperm donor is known as donor sperm.
The British Pregnancy Advisory Service (BPAS) is a British charity whose stated purpose is to avoid unwanted pregnancy by advocating and providing high quality, affordable services to prevent or end unwanted pregnancies with contraception or by abortion."
Jane Denton,, is a United Kingdom nurse and midwife notable for her contributions to fertility nursing and genetics. She was made a Fellow of the Royal College of Nursing in 2006.

Reproductive medicine is a branch of medicine concerning the male and female reproductive systems. It encompasses a variety of reproductive conditions, their prevention and assessment, as well as their subsequent treatment and prognosis.
Sammy Lee was an expert on fertility and in vitro fertilisation
Evans v. the United Kingdom was a key case at the European Court of Human Rights. The case outcome could have had a major impact on fertility law, not only within the United Kingdom but also the other Council of Europe countries.

The Human Fertilisation and Embryology Act 1990 is an Act of the Parliament of the United Kingdom. It created the Human Fertilisation and Embryology Authority which is in charge of human embryo research, along with monitoring and licensing fertility clinics in the United Kingdom.
Donor registration facilitates donor conceived people, sperm donors and egg donors to establish contact with genetic kindred. Registries are mostly used by donor conceived people to find out their genetic heritage and to find half-siblings from the same egg or sperm donor. In some jurisdictions donor registration is compulsory, while in others it is voluntary; but most jurisdictions do not have any registration system.
Sperm donation laws vary by country. Most countries have laws to cover sperm donations which, for example, place limits on how many children a sperm donor may give rise to, or which limit or prohibit the use of donor semen after the donor has died, or payment to sperm donors. Other laws may restrict use of donor sperm for in vitro fertilisation (IVF) treatment, which may itself be banned or restricted in some way, such as to married heterosexual couples, banning such treatment to single women or lesbian couples. Donated sperm may be used for insemination or as part of IVF treatment. Notwithstanding such laws, informal and private sperm donations take place, which are largely unregulated.
The Centre for Human Reproductive Science was established in December 2006 to further develop research and innovation in fertility diagnosis and treatment, working in partnership as the academic and research wing of the Birmingham Women's Fertility Centre at Birmingham Women’s Hospital and the University of Birmingham Medical School. A particular emphasis in the biomedical research strategy is placing research and discovery in the true physiological context.
Fertility tourism is the practice of traveling to another country or jurisdiction for fertility treatment, and may be regarded as a form of medical tourism. A person who can become pregnant is considered to have fertility issues if they are unable to have a clinical pregnancy after 12 months of unprotected intercourse. Infertility, or the inability to get pregnant, affects about 8-12% of couples looking to conceive or 186 million people globally. In some places, rates of infertility surpass the global average and can go up to 30% depending on the country. Areas with lack of resources, such as assisted reproductive technologies (ARTs), tend to correlate with the highest rates of infertility.
Sperm donation is the provision by a man of his sperm with the intention that it be used in the artificial insemination or other "fertility treatment" of one or more women who are not his sexual partners in order that they may become pregnant by him. Where pregnancies go to full term, the sperm donor will be the biological father of every baby born from his donations. The man is known as a sperm donor and the sperm he provides is known as "donor sperm" because the intention is that the man will give up all legal rights to any child produced from his sperm, and will not be the legal father. Sperm donation may also be known as "semen donation".

The Human Fertilisation and Embryology Act 2008 is an Act of the Parliament of the United Kingdom. The Act constitutes a major review and update of the Human Fertilisation and Embryology Act 1990.
Mitochondrial replacement therapy (MRT), sometimes called mitochondrial donation, is the replacement of mitochondria in one or more cells to prevent or ameliorate disease. MRT originated as a special form of in vitro fertilisation in which some or all of the future baby's mitochondrial DNA (mtDNA) comes from a third party. This technique is used in cases when mothers carry genes for mitochondrial diseases. The therapy is approved for use in the United Kingdom. A second application is to use autologous mitochondria to replace mitochondria in damaged tissue to restore the tissue to a functional state. This has been used in clinical research in the United States to treat cardiac-compromised newborns.
Partner-assisted reproduction, reception of oocytes from partner (ROPA), reciprocal IVF,shared motherhood, partner IVF or co-IVF is a method of family building that is used by couples who both possess female reproductive organs. The method uses in vitro fertilization (IVF), a method that means eggs are removed from the ovaries, fertilized in a laboratory, and then one or more of the resulting embryos are placed in the uterus to hopefully create a pregnancy. Reciprocal IVF differs from standard IVF in that two partners are involved: the eggs are taken from one partner, and the other partner carries the pregnancy. In this way, the process is mechanically identical to IVF with egg donation. Reciprocal IVF offers the highest chance for pregnancy and a lower chance of a multiple births.
Simon Fishel is an English physiologist, biochemist and pioneering in vitro fertilisation (IVF) specialist.

Kamal Kishore Ahuja is a physiologist and the managing and scientific director of JD Healthcare, the holding company for The London Women's Clinic, The London Ultrasound Centre, The London Sperm Bank, The London Egg Bank and the Bridge Centre. He was a pioneer of egg sharing in the UK in the 1990s and released an app to help women search for donor sperm in 2016.