A computed tomography scan is a medical imaging technique used to obtain detailed internal images of the body. The personnel that perform CT scans are called radiographers or radiology technologists.

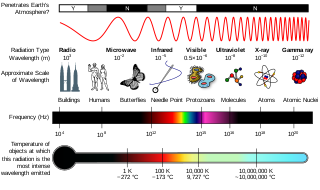
Radiography is an imaging technique using X-rays, gamma rays, or similar ionizing radiation and non-ionizing radiation to view the internal form of an object. Applications of radiography include medical and industrial radiography. Similar techniques are used in airport security,. To create an image in conventional radiography, a beam of X-rays is produced by an X-ray generator and it is projected towards the object. A certain amount of the X-rays or other radiation are absorbed by the object, dependent on the object's density and structural composition. The X-rays that pass through the object are captured behind the object by a detector. The generation of flat two-dimensional images by this technique is called projectional radiography. In computed tomography, an X-ray source and its associated detectors rotate around the subject, which itself moves through the conical X-ray beam produced. Any given point within the subject is crossed from many directions by many different beams at different times. Information regarding the attenuation of these beams is collated and subjected to computation to generate two-dimensional images on three planes which can be further processed to produce a three-dimensional image.
Medical physics deals with the application of the concepts and methods of physics to the prevention, diagnosis and treatment of human diseases with a specific goal of improving human health and well-being. Since 2008, medical physics has been included as a health profession according to International Standard Classification of Occupation of the International Labour Organization.
Radiation protection, also known as radiological protection, is defined by the International Atomic Energy Agency (IAEA) as "The protection of people from harmful effects of exposure to ionizing radiation, and the means for achieving this". Exposure can be from a source of radiation external to the human body or due to internal irradiation caused by the ingestion of radioactive contamination.

Nuclear medicine, or nucleology, is a medical specialty involving the application of radioactive substances in the diagnosis and treatment of disease. Nuclear imaging is, in a sense, radiology done inside out, because it records radiation emitted from within the body rather than radiation that is transmitted through the body from external sources like X-ray generators. In addition, nuclear medicine scans differ from radiology, as the emphasis is not on imaging anatomy, but on the function. For such reason, it is called a physiological imaging modality. Single photon emission computed tomography (SPECT) and positron emission tomography (PET) scans are the two most common imaging modalities in nuclear medicine.

Health physics, also referred to as the science of radiation protection, is the profession devoted to protecting people and their environment from potential radiation hazards, while making it possible to enjoy the beneficial uses of radiation. Health physicists normally require a four-year bachelor’s degree and qualifying experience that demonstrates a professional knowledge of the theory and application of radiation protection principles and closely related sciences. Health physicists principally work at facilities where radionuclides or other sources of ionizing radiation are used or produced; these include research, industry, education, medical facilities, nuclear power, military, environmental protection, enforcement of government regulations, and decontamination and decommissioning—the combination of education and experience for health physicists depends on the specific field in which the health physicist is engaged.

Radioactive contamination, also called radiological pollution, is the deposition of, or presence of radioactive substances on surfaces or within solids, liquids, or gases, where their presence is unintended or undesirable.
In radiation physics, kerma is an acronym for "kinetic energy released per unit mass", defined as the sum of the initial kinetic energies of all the charged particles liberated by uncharged ionizing radiation in a sample of matter, divided by the mass of the sample. It is defined by the quotient .

Iodine-131 is an important radioisotope of iodine discovered by Glenn Seaborg and John Livingood in 1938 at the University of California, Berkeley. It has a radioactive decay half-life of about eight days. It is associated with nuclear energy, medical diagnostic and treatment procedures, and natural gas production. It also plays a major role as a radioactive isotope present in nuclear fission products, and was a significant contributor to the health hazards from open-air atomic bomb testing in the 1950s, and from the Chernobyl disaster, as well as being a large fraction of the contamination hazard in the first weeks in the Fukushima nuclear crisis. This is because 131I is a major fission product of uranium and plutonium, comprising nearly 3% of the total products of fission. See fission product yield for a comparison with other radioactive fission products. 131I is also a major fission product of uranium-233, produced from thorium.
The International Commission on Radiological Protection (ICRP) is an independent, international, non-governmental organization, with the mission to protect people, animals, and the environment from the harmful effects of ionising radiation. Its recommendations form the basis of radiological protection policy, regulations, guidelines and practice worldwide.
Radiobiology is a field of clinical and basic medical sciences that involves the study of the effects of ionizing radiation on living things, in particular health effects of radiation. Ionizing radiation is generally harmful and potentially lethal to living things but can have health benefits in radiation therapy for the treatment of cancer and thyrotoxicosis. Its most common impact is the induction of cancer with a latent period of years or decades after exposure. High doses can cause visually dramatic radiation burns, and/or rapid fatality through acute radiation syndrome. Controlled doses are used for medical imaging and radiotherapy.

The International Organization for Medical Physics (IOMP) is a professional organization for medical physics with nearly 22,000 members in 84 countries.
Cumulative dose is the total dose resulting from repeated exposures of ionizing radiation to an occupationally exposed worker to the same portion of the body, or to the whole body, over a period of time.
Patients are exposed to ionizing radiation when they undergo diagnostic examinations using x-rays or radiopharmaceuticals. Radiation emitted by radioisotopes or radiation generators is utilized in therapy for cancer or benign lesions and also in interventional procedures using fluoroscopy. There has been a tremendous increase in the use of ionizing radiation in medicine during recent decades and health professionals and patients are concerned about the harmful effects of radiation. The International Atomic Energy Agency (IAEA) has established a program on radiological protection of patients in recognition of the increasing importance of this topic. The emphasis in the past had been on radiation protection of staff and this has helped to reduce radiation doses to staff at levels well below the limits prescribed by the International Commission on Radiological Protection (ICRP) and accepted by most countries. The recent emphasis on radiation protection of patients is helping in developing strategies to reduce radiation doses to patients without compromising on diagnostic or therapeutic purpose.
Paediatric radiology is a subspecialty of radiology involving the imaging of fetuses, infants, children, adolescents and young adults. Many paediatric radiologists practice at children's hospitals.
Computational human phantoms are models of the human body used in computerized analysis. Since the 1960s, the radiological science community has developed and applied these models for ionizing radiation dosimetry studies. These models have become increasingly accurate with respect to the internal structure of the human body.
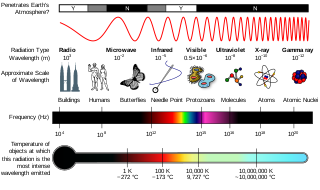
Radiation exposure is a measure of the ionization of air due to ionizing radiation from photons. It is defined as the electric charge freed by such radiation in a specified volume of air divided by the mass of that air. As of 2007, "medical radiation exposure" was defined by the International Commission on Radiological Protection as exposure incurred by people as part of their own medical or dental diagnosis or treatment; by persons, other than those occupationally exposed, knowingly, while voluntarily helping in the support and comfort of patients; and by volunteers in a programme of biomedical research involving their exposure. Common medical tests and treatments involving radiation include X-rays, CT scans, mammography, lung ventilation and perfusion scans, bone scans, cardiac perfusion scan, angiography, radiation therapy, and more. Each type of test carries its own amount of radiation exposure. There are two general categories of adverse health effects caused by radiation exposure: deterministic effects and stochastic effects. Deterministic effects are due to the killing/malfunction of cells following high doses; and stochastic effects involve either cancer development in exposed individuals caused by mutation of somatic cells, or heritable disease in their offspring from mutation of reproductive (germ) cells.
The European Federation of Organisations for Medical Physics (EFOMP) was founded in May 1980 in London to serve as an umbrella organisation representing the national Medical Physics societies in Europe. The office moved to Utrecht in January 2021. It is a non-profit organisation and aims to foster and coordinate the activities of its national member organisations, encourage exchange and dissemination of professional and scientific information, develop guidelines for education, training and accreditation programmes and to make recommendations on the responsibilities, organisational relationships and roles of medical physicists.
Caridad Borrás is a Spanish medical physicist. Her career started in 1964 at the Santa Creu i Sant Pau Hospital in Barcelona. From 1988 to 2000, she was Regional Advisor of the Radiological Health Program and, from 2000 to 2002, Coordinator of Essential Drugs and Technology at the Pan American Health Organization in Washington D.C.

Flight-time equivalent dose (FED) is an informal unit of measurement of ionizing radiation exposure. Expressed in units of flight-time, one unit of flight-time is approximately equivalent to the radiological dose received during the same unit of time spent in an airliner at cruising altitude. FED is intended as a general educational unit to enable a better understanding of radiological dose by converting dose typically presented in sieverts into units of time. FED is only meant as an educational exercise and is not a formally adopted dose measurement.