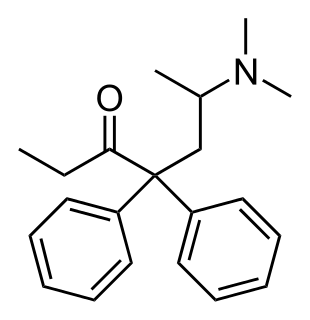
Methadone, sold under the brand names Dolophine and Methadose among others, is a synthetic opioid agonist used for opioid maintenance therapy in opioid dependence and for chronic pain management. It is most commonly used in the treatment of addiction to heroin. Detoxification using methadone can be accomplished in less than a month, or it may be done gradually over as long as six months. While a single dose has a rapid effect, maximum effect can take up to five days of use. The pain-relieving effects last about six hours after a single dose. After long-term use, in people with normal liver function, effects last 8 to 36 hours. Methadone is usually taken by mouth and rarely by injection into a muscle or vein.

Opioid use disorder (OUD) is a substance use disorder relating to the use of an opioid. Any such disorder causes significant impairment or distress. Signs of the disorder include a strong desire to use opioids, increased tolerance to opioids, difficulty fulfilling obligations, trouble reducing use, and withdrawal symptoms with discontinuation. Opioid withdrawal symptoms may include nausea, muscle aches, diarrhea, trouble sleeping, agitation, and a low mood. Addiction and dependence are components of a substance use disorder. Complications may include opioid overdose, suicide, HIV/AIDS, hepatitis C, and problems at school, work, or home.

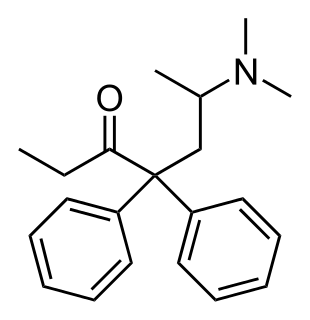
Buprenorphine is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, it is typically started when withdrawal symptoms have begun and for the first two days of treatment under direct observation of a health-care provider. The combination formulation of buprenorphine/naloxone (Suboxone) is recommended to discourage misuse by injection. Maximum pain relief is generally within an hour with effects up to 24 hours.
A methadone clinic, or substance use disorder services clinic (SUDS), is a clinic which has been established for the dispensing of medications used in the treatment of opiate dependence —historically and most commonly methadone, although buprenorphine is also increasingly prescribed. Medically assisted drug therapy treatment is indicated in patients who are opioid-dependent or have a history of opioid dependence. Methadone is a schedule II (USA) opioid analgesic, that is also prescribed for pain management. It is a long-acting opioid that can delay the opioid withdrawal symptoms that patients experience from taking short-acting opioids, like heroin, and allow time for detoxification. In the United States, by law, patients must receive methadone under the supervision of a physician, and dispensed through an opioid treatment program certified by Substance Abuse and Mental Health Services Administration and registered with the Drug Enforcement Administration.
Vincent Dole was an American doctor, who, along with his wife, Marie Nyswander, developed the use of methadone to treat heroin addiction. Dole and Nyswander, in establishing methadone maintenance treatment (MMT), improved treatment options in addiction medicine which for a century had been based on the conventional view that narcotic addiction was the result of an intractable moral defect. His work resulted in the partial re-legalization of opioid maintenance in the United States. For this contribution he was a recipient of the 1988 Albert Lasker Award for Clinical Medical Research.

An opioid overdose is toxicity due to excessive consumption of opioids, such as morphine, heroin, fentanyl, tramadol, and methadone. This preventable pathology can be fatal if it leads to respiratory depression, a lethal condition that can cause hypoxia. Other symptoms include insufficient breathing, small pupils, and unconsciousness, however its onset can depend on the method of ingestion, the dosage and individual risk factors. Although there were over 110,000 deaths in 2017 due to opioids, individuals who survived also faced adverse complications, including permanent brain damage.

Heroin-assisted treatment (HAT), or diamorphine assisted treatment, refers to the prescribing of semi-synthetic heroin to opiate addicts who do not benefit from or cannot tolerate treatment with one of the established drugs used in opiate replacement therapy like methadone or buprenorphine. For this group of patients, heroin-assisted treatment has proven superior in improving their social and health situation. It has also been shown to save money, as it significantly reduces costs incurred by trials, incarceration, health interventions and delinquency. It has also drastically reduced overdose deaths in the countries utilizing it, as patients take their dose in a controlled, professionally supervised setting, and Narcan (naloxone) is on hand in the case of an accidental overdose. Opiate related overdoses in the U.S. kill around 70,000 people per year.
Marie Nyswander was an American psychiatrist and psychoanalyst known for developing and popularizing the use of methadone to treat heroin addiction.
Mark S. Gold is an American physician, professor, author, and researcher on the effects of opioids, cocaine, tobacco, and other drugs as well as food on the brain and behavior.
Methadone maintenance treatment is the use of methadone, administered over a prolonged period of time, as treatment for someone who is addicted to opioids such as heroin, where detoxification has been unsuccessful and/or admittance to a substance abuse treatment facility requires complete abstinence. "Methadone maintenance makes possible a first step toward social rehabilitation" because it allows addicts to avoid the uncomfortable withdrawal symptoms that result from complete abstinence. Methadone maintenance can also be used for patients who suffer with severe pain problems that are resistant to other drugs.
Martin T. Schechter is a Canadian epidemiologist recognized for contributions to HIV research, prevention and treatments and to addiction research. He is a professor and the former founding director of the School of Population and Public Health in the Faculty of Medicine at the University of British Columbia (UBC). Schechter received his Order of British Columbia in 1994 alongside BC's first Nobel Prize laureate Michael Smith. He now serves as Chief Scientific Officer of the Michael Smith Foundation for Health Research.

Buprenorphine/naloxone, sold under the brand name Suboxone among others, is a fixed-dose combination medication that includes buprenorphine and naloxone. It is used to treat opioid use disorder, and reduces the mortality of opioid use disorder by 50%. It relieves cravings to use and withdrawal symptoms. Buprenorphine/naloxone is available for use in two different forms, under the tongue or in the cheek.

Yasmin Hurd is the Ward-Coleman Chair of Translational Neuroscience and the Director of the Addiction Institute, where Hurd is the only Black tenure-track basic science professor at Mount Sinai. Hurd holds appointments as faculty of Neuroscience, Psychiatry, Pharmacology and Systems Therapeutics at the Icahn School of Medicine at Mount Sinai in New York City and is globally recognized for her translational research on the underlying neurobiology of substance use disorders and comorbid psychiatric disorders. Hurd's research on the transgenerational effects of early cannabis exposure on the developing brain and behavior and on the therapeutic properties of marijuana has garnered substantial media attention.

Mary Jeanne Kreek was an American neurobiologist specializing in the study and treatment of addiction. She is best known for her work with Marie Nyswander and Dr. Vincent Dole in the development of methadone therapy for heroin addiction.

The opioid epidemic refers to the extensive overuse of opioid medications, both from medical prescriptions and from illegal sources. The epidemic began in the United States in the late 1990s, according to the Centers for Disease Control and Prevention (CDC), when opioids were increasingly prescribed for pain management and resulted in a rise in overall opioid use throughout subsequent years. Use of opioids constitutes a public health emergency. The great majority of Americans who use prescription opioids do not believe that they are misusing them.
Robert G. Newman was an American physician, scientist, health manager and philanthropist.
Chinazo D. Opia Cunningham is a physician, researcher, and Professor of Medicine at Albert Einstein College of Medicine in New York City. She is also the Director of Diversity Affairs for the Department of Medicine. She worked on the frontlines during the HIV/AIDS crisis in San Francisco and in 2020 began working on the frontlines of the Coronavirus disease 2019 (COVID-19) pandemic in New York City. She also specializes in treating patients with addiction, overseeing a network using buprenorphine to treat people with opioid addiction.
Aslam Anis is a Bangladeshi-Canadian health economist whose primary areas of research involvement include health services research, measuring patient-reported outcomes, Canadian competition policy in the pharmaceutical industry, and the cost-effectiveness of treatments for HIV/AIDS, rheumatoid arthritis, and other conditions.
Kelly J. Clark is an American physician and psychiatrist known for her work in the fields of substance use disorder, addiction medicine, and addiction psychiatry.
Opioid agonist therapy (OAT) is a treatment where prescribed opioid agonists are given to patients who live with opioid addiction. The benefits of this treatment include a more manageable withdrawal experience, cognitive improvement, and lower HIV transmission. The length of OAT varies per person based on their biology, environmental surroundings, and quality of life.