Related Research Articles
Occupational therapists (OTs) are health care professionals specializing in occupational therapy and occupational science. OTs and occupational therapy assistants (OTAs) use scientific bases and a holistic perspective to promote a person's ability to fulfill their daily routines and roles. OTs have training in the physical, psychological, and social aspects of human functioning deriving from an education grounded in anatomical and physiological concepts, and psychological perspectives. They enable individuals across the lifespan by optimizing their abilities to perform activities that are meaningful to them ("occupations"). Human occupations include activities of daily living, work/vocation, play, education, leisure, rest and sleep, and social participation.

Health care, or healthcare, is the improvement of health via the prevention, diagnosis, treatment, amelioration or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals and allied health fields. Medicine, dentistry, pharmacy, midwifery, nursing, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training, and other health professions all constitute health care. The term includes work done in providing primary care, secondary care, tertiary care, and public health.

Ambulatory care or outpatient care is medical care provided on an outpatient basis, including diagnosis, observation, consultation, treatment, intervention, and rehabilitation services. This care can include advanced medical technology and procedures even when provided outside of hospitals.

Occupational therapy (OT) is a healthcare profession that involves the use of assessment, intervention, consultation, and coaching to develop, recover, or maintain meaningful occupations of individuals, groups, or communities. The field of OT consists of health care practitioners trained and educated to support mental health and physical performance. Occupational therapists specialize in teaching, educating, and supporting participation in activities that occupy an individual's time. It is an independent health profession sometimes categorized as an allied health profession and consists of occupational therapists (OTs) and occupational therapy assistants (OTAs). OTs and OTAs have different roles, with OTs licensed to complete comprehensive occupational therapy evaluations. Both professionals work with people who want to improve their ability to participate in meaningful occupations.
The National Alliance on Mental Illness (NAMI) is a United States-based nonprofit organization originally founded as a grassroots group by family members of people diagnosed with mental illness. NAMI identifies its mission as "providing advocacy, education, support and public awareness so that all individuals and families affected by mental illness can build better lives" and its vision as "a world where all people affected by mental illness live healthy, fulfilling lives supported by a community that cares". NAMI offers classes and trainings for people living with mental illnesses, their families, community members, and professionals, including what is termed psychoeducation, or education about mental illness. NAMI holds regular events which combine fundraising for the organization and education, including Mental Illness Awareness Week and NAMIWalks.
General practice is personal, family, and community-orientated comprehensive primary care that includes diagnosis, continues over time and is anticipatory as well as responsive.

Mental health encompasses emotional, psychological, and social well-being, influencing cognition, perception, and behavior. According to World Health Organization (WHO), it is a "state of well-being in which the individual realizes his or her abilities, can cope with the normal stresses of life, can work productively and fruitfully, and can contribute to his or her community". It likewise determines how an individual handles stress, interpersonal relationships, and decision-making. Mental health includes subjective well-being, perceived self-efficacy, autonomy, competence, intergenerational dependence, and self-actualization of one's intellectual and emotional potential, among others. From the perspectives of positive psychology or holism, mental health may include an individual's ability to enjoy life and to create a balance between life activities and efforts to achieve psychological resilience. Cultural differences, personal philosophy, subjective assessments, and competing professional theories all affect how one defines "mental health". Some early signs related to mental health difficulties are sleep irritation, lack of energy, lack of appetite, thinking of harming oneself or others, self-isolating, and frequently zoning out.
Online counseling or online therapy is a form of professional mental health counseling that is generally performed through the internet. Computer aided technologies are used by the trained professional counselors and individuals seeking counseling services to communicate rather than conventional face-to-face interactions. Online counseling is also referred to as teletherapy, e-therapy, cyber therapy, or web counseling. Services are typically offered via email, real-time chat, and video conferencing. Some clients use online counseling in conjunction with traditional psychotherapy, or nutritional counseling. An increasing number of clients are using online counseling as a replacement for office visits.
Kendra's Law, effective since November 1999, is a New York State law concerning involuntary outpatient commitment also known as assisted outpatient treatment. It grants judges the authority to issue orders that require people who meet certain criteria to regularly undergo psychiatric treatment. Failure to comply could result in commitment for up to 72 hours. Kendra's Law does not mandate that patients be forced to take medication.

The Community Mental Health Act of 1963 (CMHA) was an act to provide federal funding for community mental health centers and research facilities in the United States. This legislation was passed as part of John F. Kennedy's New Frontier. It led to considerable deinstitutionalization.
Psychiatric and mental health nurses in the U.S. Army Nurse Corps employing groundbreaking protocols and treatments in psychiatric issues to address the unique challenges that our service men and women face, more commonly post-traumatic stress disorder and traumatic brain injuries. Most people understand that trauma exposure is a popular occupational hazard for military members. Psychiatric screenings, before and during their enlistment, and treatments after being exposed to warfare, death, destruction, and torture have been extremely beneficial for military personnel and their dependents.
A mental health professional is a health care practitioner or social and human services provider who offers services for the purpose of improving an individual's mental health or to treat mental disorders. This broad category was developed as a name for community personnel who worked in the new community mental health agencies begun in the 1970s to assist individuals moving from state hospitals, to prevent admissions, and to provide support in homes, jobs, education, and community. These individuals were the forefront brigade to develop the community programs, which today may be referred to by names such as supported housing, psychiatric rehabilitation, supported or transitional employment, sheltered workshops, supported education, daily living skills, affirmative industries, dual diagnosis treatment, individual and family psychoeducation, adult day care, foster care, family services and mental health counseling.

Pine Rest Christian Mental Health Services is a psychiatric hospital and behavioral health provider, with the main treatment campus located in Grand Rapids, Michigan, Michigan. The Chief Executive Officer and President is Dr. Mark Eastburg, appointed December, 2006.
Case management is a managed care technique within the health care coverage system of the United States. It involves an integrated system that manages the delivery of comprehensive healthcare services for enrolled patients. Case managers are employed in almost every aspect of health care and these employ different approaches in the control of clinical actions.
Ambulatory care nursing is the nursing care of patients who receive treatment on an outpatient basis, ie they do not require admission to a hospital for an overnight stay. Ambulatory care includes those clinical, organizational and professional activities engaged in by registered nurses with and for individuals, groups, and populations who seek assistance with improving health and/or seek care for health-related problems. The American Academy of Ambulatory Care Nursing (AAACN) describes ambulatory care nursing as a comprehensive practice which is built on a broad knowledge base of nursing and health sciences, and applies clinical expertise rooted in the nursing process.
Services for mental health disorders provide treatment, support, or advocacy to people who have psychiatric illnesses. These may include medical, behavioral, social, and legal services.

The Utah State Hospital (USH) is a mental hospital located in eastern Provo, Utah. The current superintendent is Dallas Earnshaw.

Cultural competence in healthcare refers to the ability for healthcare professionals to demonstrate cultural competence toward patients with diverse values, beliefs, and feelings. This process includes consideration of the individual social, cultural, and psychological needs of patients for effective cross-cultural communication with their health care providers. The goal of cultural competence in health care is to reduce health disparities and to provide optimal care to patients regardless of their race, gender, ethnic background, native languages spoken, and religious or cultural beliefs. Cultural competency training is important in health care fields where human interaction is common, including medicine, nursing, allied health, mental health, social work, pharmacy, oral health, and public health fields.
Mark S. Komrad is an American psychiatrist on the clinical and teaching staff of the Johns Hopkins Hospital in Baltimore. He is the author of You Need Help: A Step-by-Step Plan to Convince Your Loved One to Get Counseling.
Coordinated Specialty Care (CSC) is a recovery-oriented treatment program designed for people with first episode psychosis (FEP). CSC consists of collaborative treatment planning between the client and the client's care team, consisting of mental health clinicians, psychiatrists, and case managers. CSC includes individual and family therapy, medication management, psychoeducation and support, case management, and support surrounding education and employment goals. The program is considered an early psychosis intervention and is intended to be used shortly after symptoms onset.
References
- 1 2 "Mental Health Patient Navigator". CAP Services. Archived from the original on 6 October 2014. Retrieved 7 October 2014.
- 1 2 "Navigation Services". Mental Health Partners. Retrieved 7 October 2014.
- ↑ "Navigating the System". The Kim Foundation. Archived from the original on 7 October 2014. Retrieved 7 October 2014.
- 1 2 "Health Services Consultations". Merritt Mental Health. Retrieved 7 October 2014.
- ↑ Department of Behavioral Health and Developmental Services (Commonwealth of Virginia); NAMI Virginia (20 May 2013). "Navigating the System: A Guide to Accessing Mental Health Services in Virginia" (PDF). NAMI Virginia. Archived from the original (PDF) on 6 October 2014. Retrieved 2 October 2014.
- ↑ "Navigation Services". Jefferson Center for Mental Health. Retrieved 2 October 2014.
- ↑ Napa County Health and Human Services Agency. "System Navigators". County of Napa. County of Napa, CA. Archived from the original on 6 October 2014. Retrieved 2 October 2014.
- ↑ Goldberg, Leslie S. (23 August 2009). "Educational Consultant Services (Crystal Ball Not Included)". Educational Consulting Blog. The Goldberg Center for Educational Planning.
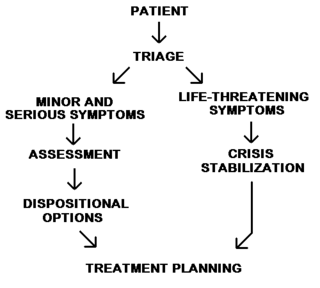
- 1 2 3 4 "The Model". MerrittMentalHealth.com. Merritt Mental Health. Retrieved 7 October 2014.