Related Research Articles

A pharmacist, also known as a chemist in Commonwealth English, is a healthcare professional who is knowledgeable about preparation, mechanism of action, clinical usage and legislation of medications in order to dispense them safely to the public and to provide consultancy services. A pharmacist also often serves as a primary care provider in the community and offers services, such as health screenings and immunizations.

Pharmacy is the science and practice of discovering, producing, preparing, dispensing, reviewing and monitoring medications, aiming to ensure the safe, effective, and affordable use of medicines. It is a miscellaneous science as it links health sciences with pharmaceutical sciences and natural sciences. The professional practice is becoming more clinically oriented as most of the drugs are now manufactured by pharmaceutical industries. Based on the setting, pharmacy practice is either classified as community or institutional pharmacy. Providing direct patient care in the community of institutional pharmacies is considered clinical pharmacy.

A prescription, often abbreviated ℞ or Rx, is a formal communication from a physician or other registered healthcare professional to a pharmacist, authorizing them to dispense a specific prescription drug for a specific patient. Historically, it was a physician's instruction to an apothecary listing the materials to be compounded into a treatment—the symbol ℞ comes from the first word of a medieval prescription, Latin recipere, that gave the list of the materials to be compounded.
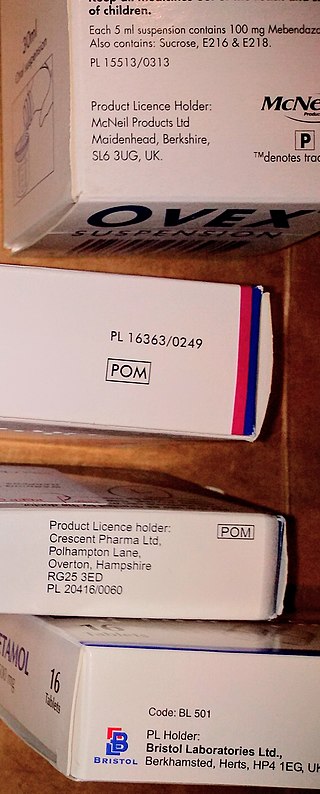
A prescription drug is a pharmaceutical drug that is permitted to be dispensed only to those with a medical prescription. In contrast, over-the-counter drugs can be obtained without a prescription. The reason for this difference in substance control is the potential scope of misuse, from drug abuse to practicing medicine without a license and without sufficient education. Different jurisdictions have different definitions of what constitutes a prescription drug.

NHS Digital was the trading name of the Health and Social Care Information Centre, which was the national provider of information, data and IT systems for commissioners, analysts and clinicians in health and social care in England, particularly those involved with the National Health Service of England. The organisation was an executive non-departmental public body of the Department of Health and Social Care.

NHS Scotland, sometimes styled NHSScotland, is the publicly–funded healthcare system in Scotland and one of the four systems that make up the National Health Service in the United Kingdom. It operates 14 territorial NHS boards across Scotland, supported by seven special non-geographic health boards, and Public Health Scotland.
An online pharmacy, internet pharmacy, or mail-order pharmacy is a pharmacy that operates over the Internet and sends orders to customers through mail, shipping companies, or online pharmacy web portal.
The NHS treatments blacklist is an informal name for a list of medicines and procedures which will not be funded by public money except in exceptional cases. These include but are not limited to procedures which the National Institute for Health and Care Excellence (NICE) has ruled of limited effectiveness and particular brand name medicines. In 2017 there was a proposal for 3,200 over-the-counter (OTC) drugs to be restricted and 18 procedures to be added to the list. This generated some controversy amongst doctors with some arguing that OTC should be blacklisted instead, and others believing the move did not take into account individual patient needs.
Charges for prescriptions for medicines and some medical appliances are payable by adults in England under the age of 60. However, people may be exempt from charges in various exemption categories. Charges were abolished by NHS Wales in 2007, Health and Social Care in Northern Ireland in 2010 and by NHS Scotland in 2011. In 2010/11, in England, £450 million was raised through these charges, some 0.5% of the total NHS budget. In April 2021 the charge was raised to £9.35 for up to a three-month supply of each item. In 2022, for the first time since 2010, the charge was not increased.
The term private prescription is a term used in the United Kingdom for a medical prescription which is not supplied under the National Health Service (NHS).

A pharmacy is a premises which provides pharmaceutical drugs, among other products. At the pharmacy, a pharmacist oversees the fulfillment of medical prescriptions and is available to counsel patients about prescription and over-the-counter drugs or about health problems and wellness issues. A typical pharmacy would be in the commercial area of a community.
SystmOne is a centrally hosted clinical computer system developed by Horsforth-based The Phoenix Partnership (TPP). It is used by healthcare professionals in the UK predominantly in primary care. The system is being deployed as one of the accredited systems in the government's programme of modernising IT in the NHS.

Healthcare in Wales is mainly provided by the Welsh public health service, NHS Wales. NHS Wales provides healthcare to all permanent residents that is free at the point of need and paid for from general taxation. Health is a matter that is devolved, and considerable differences are now developing between the public healthcare systems in the different countries of the United Kingdom, collectively the National Health Service (NHS). Though the public system dominates healthcare provision, private health care and a wide variety of alternative and complementary treatments are available for those willing to pay.
A formulary is a list of pharmaceutical drugs, often decided upon by a group of people, for various reasons such as insurance coverage or use at a medical facility. Traditionally, a formulary contained a collection of formulas for the compounding and testing of medication. Today, the main function of a prescription formulary is to specify particular medications that are approved to be prescribed at a particular hospital, in a particular health system, or under a particular health insurance policy. The development of prescription formularies is based on evaluations of efficacy, safety, and cost-effectiveness of drugs.
Electronic prescription is the computer-based electronic generation, transmission, and filling of a medical prescription, taking the place of paper and faxed prescriptions. E-prescribing allows a physician, physician assistant, pharmacist, or nurse practitioner to use digital prescription software to electronically transmit a new prescription or renewal authorization to a community or mail-order pharmacy. It outlines the ability to send error-free, accurate, and understandable prescriptions electronically from the healthcare provider to the pharmacy. E-prescribing is meant to reduce the risks associated with traditional prescription script writing. It is also one of the major reasons for the push for electronic medical records. By sharing medical prescription information, e-prescribing seeks to connect the patient's team of healthcare providers to facilitate knowledgeable decision making.
Pharmacy2U is a British online pharmacy company, which manages NHS repeat prescriptions on behalf of patients.
EMIS Health, formerly known as Egton Medical Information Systems, supplies electronic patient record systems and software used in primary care, acute care and community pharmacy in the United Kingdom. The company is based in Leeds. It claims that more than half of GP practices across the UK use EMIS Health software and holds number one or two market positions in its main markets. In June 2022 the company was acquired by Bordeaux UK Holdings II Limited, an affiliate of UnitedHealth's Optum business for a 49% premium on EMIS's closing share price.
Pharmacy in the United Kingdom has been an integral part of the National Health Service since it was established in 1948. Unlike the rest of the NHS, pharmacies are largely privately provided apart from those in hospitals, and even these are now often privately run.
In 2005 the National Health Service (NHS) in the United Kingdom began deployment of electronic health record systems in NHS Trusts. The goal was to have all patients with a centralized electronic health record by 2010. Lorenzo patient record systems were adopted in a number of NHS trusts. While many hospitals acquired electronic patient records systems in this process, there was no national healthcare information exchange. Ultimately, the program was dismantled after a cost to the UK taxpayer was over $24 billion, and is considered one of the most expensive healthcare IT failures.
The Australian Digital Health Agency is the Australian Government statutory agency responsible for My Health Record, Australia's digital prescriptions and health referral system, and other e-health programs under the national digital health strategy. The agency replaces the former National E-Health Transition Authority which ceased on 1 July 2016. The agency is led by its chief executive officer, board, and is subject to directions issued by the minister for health and aged care on the approval of all state and territory health ministers.
References
- ↑ NHS Connecting for Health - What is the Electronic Prescription Service?
- ↑ NHS Connecting for Health - Electronic Prescription Service - Introducing Release 1
- ↑ NHS Connecting for Health - Electronic Prescription Service - Introducing Release 2
- ↑ "Every GP surgery in London now using the Electronic Prescription Service". Pharmaceutical Journal. 9 August 2018. Retrieved 21 September 2018.
- ↑ "Electronic prescriptions to be introduced nationally from November 2019". Pharmaceutical Journal. 19 October 2019. Retrieved 8 December 2019.
- ↑ "Hospitals expected to begin testing electronic prescribing systems from autumn 2021". Pharmaceutical Journal. 28 July 2021. Retrieved 6 September 2021.
- ↑ "Acute Medication Service (AMS)". Community Pharmacy Scotland. Retrieved 16 February 2020.
- ↑ "ePrescribing: The next stage of digital healthcare". Senedd Research. 16 March 2022. Retrieved 18 November 2022.
- ↑ Neal, Ed (1 November 2022). "EPS Tracker Integration is Now Live on Healthera". Healthera. Retrieved 21 December 2022.
- ↑ E-prescription Software Guide