Related Research Articles

Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The digestive system consists of the gastrointestinal tract, sometimes referred to as the GI tract, which includes the esophagus, stomach, small intestine and large intestine as well as the accessory organs of digestion which include the pancreas, gallbladder, and liver.

Ulcerative colitis (UC) is one of the two types of inflammatory bowel disease (IBD), with the other type being Crohn's disease. It is a long-term condition that results in inflammation and ulcers of the colon and rectum. The primary symptoms of active disease are abdominal pain and diarrhea mixed with blood (hematochezia). Weight loss, fever, and anemia may also occur. Often, symptoms come on slowly and can range from mild to severe. Symptoms typically occur intermittently with periods of no symptoms between flares. Complications may include abnormal dilation of the colon (megacolon), inflammation of the eye, joints, or liver, and colon cancer.
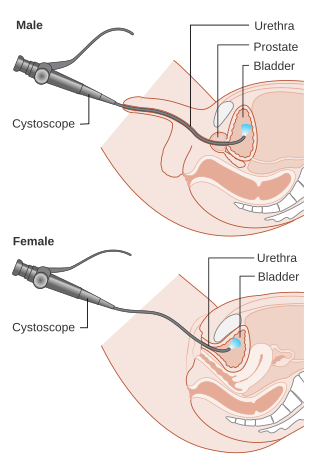
Cystoscopy is endoscopy of the urinary bladder via the urethra. It is carried out with a cystoscope.

An endoscopy is a procedure used in medicine to look inside the body. The endoscopy procedure uses an endoscope to examine the interior of a hollow organ or cavity of the body. Unlike many other medical imaging techniques, endoscopes are inserted directly into the organ.

A urethral stricture is a narrowing of the urethra, the tube connected to the bladder that allows the passing of urine. The narrowing reduces the flow of urine and makes it more difficult or even painful to empty the bladder.
An endoscope is an inspection instrument composed of image sensor, optical lens, light source and mechanical device, which is used to look deep into the body by way of openings such as the mouth or anus. A typical endoscope applies several modern technologies including optics, ergonomics, precision mechanics, electronics, and software engineering. With an endoscope, it is possible to observe lesions that cannot be detected by X-ray, making it useful in medical diagnosis. Endoscopes use tubes which are only a few millimeters thick to transfer illumination in one direction and high-resolution images in real time in the other direction, resulting in minimally invasive surgeries. It is used to examine the internal organs like the throat or esophagus. Specialized instruments are named after their target organ. Examples include the cystoscope (bladder), nephroscope (kidney), bronchoscope (bronchus), arthroscope (joints) and colonoscope (colon), and laparoscope. They can be used to examine visually and diagnose, or assist in surgery such as an arthroscopy.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.
Gastrointestinal cancer refers to malignant conditions of the gastrointestinal tract and accessory organs of digestion, including the esophagus, stomach, biliary system, pancreas, small intestine, large intestine, rectum and anus. The symptoms relate to the organ affected and can include obstruction, abnormal bleeding or other associated problems. The diagnosis often requires endoscopy, followed by biopsy of suspicious tissue. The treatment depends on the location of the tumor, as well as the type of cancer cell and whether it has invaded other tissues or spread elsewhere. These factors also determine the prognosis.
Pouchitis is an umbrella term for inflammation of the ileal pouch, an artificial rectum surgically created out of ileum in patients who have undergone a proctocolectomy or total colectomy. The ileal pouch-anal anastomosis is created in the management of patients with ulcerative colitis, indeterminate colitis, familial adenomatous polyposis, cancer, or rarely, other colitides.

A colorectal polyp is a polyp occurring on the lining of the colon or rectum. Untreated colorectal polyps can develop into colorectal cancer.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.

Chromoendoscopy is a medical procedure wherein dyes are instilled into the gastrointestinal tract at the time of visualization with fibre-optic endoscopy. The purposes of chromoendoscopy is chiefly enhance the characterization of tissues, although dyes may be used for other functional purposes. The detail achieved with chromoendoscopy can often allow for identification of the tissue type or pathology based upon the pattern uncovered.
Endoscopic mucosal resection is a technique used to remove cancerous or other abnormal lesions found in the digestive tract. It is one method of performing a mucosectomy.
Endomicroscopy is a technique for obtaining histology-like images from inside the human body in real-time, a process known as ‘optical biopsy’. It generally refers to fluorescence confocal microscopy, although multi-photon microscopy and optical coherence tomography have also been adapted for endoscopic use. Commercially available clinical and pre-clinical endomicroscopes can achieve a resolution on the order of a micrometre, have a field-of-view of several hundred µm, and are compatible with fluorophores which are excitable using 488 nm laser light. The main clinical applications are currently in imaging of the tumour margins of the brain and gastro-intestinal tract, particularly for the diagnosis and characterisation of Barrett’s Esophagus, pancreatic cysts and colorectal lesions. A number of pre-clinical and transnational applications have been developed for endomicroscopy as it enables researchers to perform live animal imaging. Major pre-clinical applications are in gastro-intestinal tract, toumour margin detection, uterine complications, ischaemia, live imaging of cartilage and tendon and organoid imaging.
Fluorescence guided surgery (FGS), also called fluorescence image-guided surgery, or in the specific case of tumor resection, fluorescence guided resection, is a medical imaging technique used to detect fluorescently labelled structures during surgery. Similarly to standard image-guided surgery, FGS has the purpose of guiding the surgical procedure and providing the surgeon of real time visualization of the operating field. When compared to other medical imaging modalities, FGS is cheaper and superior in terms of resolution and number of molecules detectable. As a drawback, penetration depth is usually very poor in the visible wavelengths, but it can reach up to 1–2 cm when excitation wavelengths in the near infrared are used.
Endoscopic endonasal surgery is a minimally invasive technique used mainly in neurosurgery and otolaryngology. A neurosurgeon or an otolaryngologist, using an endoscope that is entered through the nose, fixes or removes brain defects or tumors in the anterior skull base. Normally an otolaryngologist performs the initial stage of surgery through the nasal cavity and sphenoid bone; a neurosurgeon performs the rest of the surgery involving drilling into any cavities containing a neural organ such as the pituitary gland. The use of endoscope was first introduced in Transsphenoidal Pituitary Surgery by R Jankowsky, J Auque, C Simon et al. in 1992 G.
Endoscopic submucosal dissection (ESD) is an advanced surgical procedure using endoscopy to remove gastrointestinal tumors that have not entered the muscle layer. ESD may be done in the esophagus, stomach or colon. Application of endoscopic resection (ER) to gastrointestinal (GI) neoplasms is limited to lesions with no risk of nodal metastasis. Either polypectomy or endoscopic mucosal resection (EMR) is beneficial for patients because of its low level of invasiveness. However, to ensure the curative potential of these treatment modalities, accurate histopathologic assessment of the resected specimens is essential because the depth of invasion and lymphovascular infiltration of the tumor is associated with considerable risk for lymph node metastasis. For accurate assessment of the appropriateness of the therapy, en bloc resection is more desirable than piecemeal resection. For a reliable en bloc resection of GI neoplasms, a new method of ER called endoscopic submucosal dissection (ESD) has been developed.

Colonic ulcer can occur at any age, in children however they are rare. Most common symptoms are abdominal pain and hematochezia.

Lymphocytic esophagitis is a rare and poorly understood medical disorder involving inflammation in the esophagus. The disease is named from the primary inflammatory process, wherein lymphocytes are seen within the esophageal mucosa. Symptoms of the condition include difficulty swallowing, heartburn and food bolus obstruction. The condition was first described in 2006 by Rubio and colleagues. Initial reports questioned whether this was a true medical disorder, or whether the inflammation was secondary to another condition, such as gastroesophageal reflux disease.

Segmental colitis associated with diverticulosis (SCAD) is a condition characterized by localized inflammation in the colon, which spares the rectum and is associated with multiple sac-like protrusions or pouches in the wall of the colon (diverticulosis). Unlike diverticulitis, SCAD involves inflammation of the colon between diverticula, while sparing the diverticular orifices. SCAD may lead to abdominal pain, especially in the left lower quadrant, intermittent rectal bleeding and chronic diarrhea.
References
- ↑ Gono, Kazuhiro; Obi, Takashi; Yamaguchi, Masahiro; Ohyama, Nagaaki; Machida, Hirohisa; Sano, Yasushi; Yoshida, Shigeaki; Hamamoto, Yasuo; Endo, Takao (May 1, 2004). "Appearance of enhanced tissue features in narrow-band endoscopic imaging". Journal of Biomedical Optics. 9 (3): 568–577. doi: 10.1117/1.1695563 . PMID 15189095.
- ↑ "Achieve More with NBI". Olympus. Retrieved 4 May 2017.
- 1 2 Singh, R.; Mei, S. C.; Sethi, S. (2011). "Advanced endoscopic imaging in Barrett's oesophagus: A review on current practice". World Journal of Gastroenterology. 17 (38): 4271–4276. doi: 10.3748/wjg.v17.i38.4271 . PMC 3214701 . PMID 22090782.
- ↑ Tanaka, S.; Sano, Y. (2011). "Aim to Unify the Narrow Band Imaging (Nbi) Magnifying Classification for Colorectal Tumors: Current Status in Japan from a Summary of the Consensus Symposium in the 79th Annual Meeting of the Japan Gastroenterological Endoscopy Society". Digestive Endoscopy. 23: 131–139. doi:10.1111/j.1443-1661.2011.01106.x. PMID 21535219. S2CID 3218474.
- ↑ Efthymiou, M.; Taylor, A. C. F.; Kamm, M. A. (2011). "Cancer surveillance strategies in ulcerative colitis: The need for modernization". Inflammatory Bowel Diseases. 17 (8): 1800–1813. doi: 10.1002/ibd.21540 . PMID 21089179.
- ↑ Jichlinski, P.; Lovisa, B. (2011). "High magnification cystoscopy in the primary diagnosis of bladder tumors". Current Opinion in Urology. 21 (5): 398–402. doi:10.1097/MOU.0b013e32834956ad. PMID 21730856. S2CID 205841190.