Related Research Articles

Health economics is a branch of economics concerned with issues related to efficiency, effectiveness, value and behavior in the production and consumption of health and healthcare. Health economics is important in determining how to improve health outcomes and lifestyle patterns through interactions between individuals, healthcare providers and clinical settings. In broad terms, health economists study the functioning of healthcare systems and health-affecting behaviors such as smoking, diabetes, and obesity.

Family medicine is a medical specialty within primary care that provides continuing and comprehensive health care for the individual and family across all ages, genders, diseases, and parts of the body. The specialist, who is usually a primary care physician, is named a family physician. It is often referred to as general practice and a practitioner as a general practitioner. Historically, their role was once performed by any doctor with qualifications from a medical school and who works in the community. However, since the 1950s, family medicine / general practice has become a specialty in its own right, with specific training requirements tailored to each country. The names of the specialty emphasize its holistic nature and/or its roots in the family. It is based on knowledge of the patient in the context of the family and the community, focusing on disease prevention and health promotion. According to the World Organization of Family Doctors (WONCA), the aim of family medicine is "promoting personal, comprehensive and continuing care for the individual in the context of the family and the community". The issues of values underlying this practice are usually known as primary care ethics.

India's population in 2021 as per World Bank is 1.39 billion. Being the world's most populous country and one of its fastest-growing economies, India experiences both challenges and opportunities in context of public health. India is a hub for pharmaceutical and biotechnology industries; world-class scientists, clinical trials and hospitals yet country faces daunting public health challenges like child undernutrition, high rates of neonatal and maternal mortality, growth in noncommunicable diseases, high rates of road traffic accidents and other health related issues.
Peter Shawn Bearman is an American sociologist, notable for his contributions to the fields of adolescent health, research design, structural analysis, textual analysis, oral history and social networks. He is the Jonathan R. Cole Professor of Social Science in the Department of Sociology at Columbia University, the President of The American Assembly at Columbia University, as well as the director of the Interdisciplinary Center for Innovative Theory and Empirics (INCITE). He is also the founding director of the Institute for Social and Economic Research and Policy, and co-founding director of Columbia's Oral History Master of Arts Program, the first oral history masters program in the country. He was elected a Fellow of the American Academy of Arts and Sciences in 2008, a member of the National Academy of Sciences in 2014, a Guggenheim Fellow in 2016, and a member of the National Academy of Medicine in 2019.
The National Tuberculosis Elimination Programme (NTEP), earlier known as the Revised National Tuberculosis Control Programme (RNTCP), is the Public Health initiative of the Government of India that organizes its anti-Tuberculosis efforts. It functions as a flagship component of the National Health Mission (NHM) and provides technical and managerial leadership to anti-tuberculosis activities in the country. As per the National Strategic Plan 2017–25, the program has a vision of achieving a "TB free India",with a strategies under the broad themes of "Prevent, Detect,Treat and Build pillars for universal coverage and social protection". The program provides, various free of cost, quality tuberculosis diagnosis and treatment services across the country through the government health system.
The Ministry of Ayush, a ministry of the Government of India, is responsible for developing education, research and propagation of traditional medicine and alternative medicine systems in India. Ayush is a name devised from the names of the alternative healthcare systems covered by the ministry: ayurveda, yoga & naturopathy, Unani, Siddha, Sowa Rigpa, and homeopathy.

A community health worker (CHW) is a member of a community who provides basic health and medical care within their community, and is capable of providing preventive, promotional and rehabilitation care to that community, typically without formal education equal to that of a nurse, CHO, or doctor. They are chosen within the community to assist a train personnel community health extension worker who is train in college or schools of health. A community health extension worker (CHEW) is a specially trained professional who provides similar preventive, curative and rehabilitative health care and services to people where they live and work. CHEW are trained for three years and they graduate with a diploma, while the JCHEW are trained for two years and graduate with a certificate. Other terms for this type of health care provider include lay health worker, village health worker, community health aide, community health promoter, and health advisor.
The public healthcare system in India evolved due to a number of influences since 1947, including British influence from the colonial period. The need for an efficient and effective public health system in India is large.
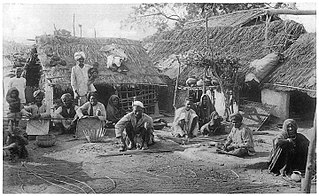
Achieving Universal Health Care has been a key goal of the Indian Government since the Constitution was drafted. The Government has since launched several programs and policies to realize ‘Health for All’ in the nation. These measures are in line with the sustainable development goals set by the United Nations. Health disparities generated through the Hindu caste system have been a major roadblock in realizing these goals. The Dalit (untouchables) community occupies the lowest stratum of the Hindu caste system. Historically, they have performed menial jobs like - manual scavenging, skinning animal hide, and sanitation. The Indian constitution officially recognizes the Dalit community as ‘Scheduled Castes’ and bans caste-based discrimination of any form. However, caste and its far-reaching effects are still prominent in several domains including healthcare. Dalits and Adivasis have the lowest healthcare utilization and outcome percentage. Their living conditions and occupations put them at high risk for disease exposure. This, clubbed with discrimination from healthcare workers and lack of awareness makes them the most disadvantaged groups in society.

India has a multi-payer universal health care model that is paid for by a combination of public and government regulated private health insurances along with the element of almost entirely tax-funded public hospitals. The public hospital system is essentially free for all Indian residents except for small, often symbolic co-payments in some services.
Dr. Kodaganur S. Gopinath, MS, FAMS, FRCS (Edin) is an Indian surgical oncologist, known for his pioneering work on oncological research. He is a recipient of many awards including Dr. B. C. Roy Award, considered to be the premier medical honour in the country. The President of India recognised his services to the field of oncology, by awarding him the fourth highest civilian award, Padma Shri, in 2010.

The Academy of Family Physicians of India (AFPI) is a professional academic society, registered as a non-profit organization in India. AFPI has been founded with the aim of promoting family medicine and primary healthcare. Family medicine is the practicing speciality and academic discipline of majority Indian doctors. Although there were GP associations such as IMA CGP and FFPAI have been existing for several decades, there was no forum for spearheading development of academic family medicine in India. AFPI is an equivalent organization to American Academy of Family Physicians, College of Family Physicians of Canada, Royal College of General Practitioners, Royal Australian College of General Practice for India.
Surinder Kumar Sama is an Indian gastroenterologist, known for his expertise in endocrinology and diabetology. He is considered by many as the Father of Gastroenterology in India. The discovery of Non-cirrhotic portal fibrosis, an idiopathic chronic liver disease is attributed to him, which he described in a 1962 medical paper, co-authored with Ramalingaswami and Wig. The Government of India awarded him the civilian honour of the Padma Shri in 2004 for his pioneering research on liver diseases including Non-cirrhotic portal fibrosis and Hepatitis B. Sama also received the highest Indian medical honour of Dr. B. C. Roy Award in 2004.
Sex education is controversial subject in India, sometimes viewed as a taboo topic; across the country and within the community, opinions on how or whether to deliver it are divided. The states of Gujarat, Maharashtra, Madhya Pradesh and Chhattisgarh have banned or refused to implement sex education in schools. The Hindu nationalist government in Madhya Pradesh said sex education had "no place in Indian culture" and plans to introduce yoga in schools instead. On the global level, India has notably fallen behind numerous countries, including underdeveloped and significantly smaller countries such as Sudan and the Congo Republic, where sex education is first taught at the primary level.
Umesh Chandra Chaturvedi was an Indian virologist, immunologist, medical microbiologist, CSIR Emeritus Scientist and a former chairman of the Bharat Immunologicals and Biologicals Corporation. The founder head of the department of microbiology at King George's Medical University, he is known for his studies on Dengue virus infection. Chaturvedi is an elected fellow of all the three major Indian science academies viz. Indian Academy of Sciences, National Academy of Sciences, India and the Indian National Science Academy as well as the Royal College of Pathologists and National Academy of Medical Sciences. The Council of Scientific and Industrial Research, the apex agency of the Government of India for scientific research, awarded him the Shanti Swarup Bhatnagar Prize for Science and Technology, one of the highest Indian science awards for his contributions to Medical Sciences in 1981.

Ayushman Bharat Pradhan Mantri Jan Arogya Yojana is a national public health insurance scheme of the Government of India that aims to provide free access to health insurance coverage for low income earners in the country. Roughly, the bottom 50% of the country qualifies for this scheme. People using the program access their own primary care services from a family doctor and when anyone needs additional care, PM-JAY provides free secondary health care for those needing specialist treatment and tertiary health care for those requiring hospitalization.

Vinod Kumar Paul is an Indian pediatrician and physician scientist currently serving as Member, NITI Aayog. He earlier served as professor of neonatology at the Department of Pediatrics, All India Institute of Medical Sciences (AIIMS), New Delhi from 1985 to 2020. He is associated with India's health policy as well as child and maternal health programs.
Neglected tropical diseases in India are a group of bacterial, parasitic, viral, and fungal infections that are common in low income countries but receive little funding to address them. Neglected tropical diseases are common in India.
Lymphatic filariasis in India refers to the presence of the disease lymphatic filariasis in India and the social response to the disease. In India, 99% of infections come from a type of mosquito spreading a type of worm through a mosquito bite. The treatment plan provides 400 million people in India with medication to eliminate the parasite. About 50 million people in India were carrying the worm as of the early 2010s, which is 40% of all the cases in the world. In collaboration with other countries around the world, India is participating in a global effort to eradicate lymphatic filariasis. If the worm is eliminated from India then the disease could be permanently eradicated. In October 2019 the Union health minister Harsh Vardhan said that India's current plan is on schedule to eradicate filariasis by 2021.

Mental healthcare in India is a right secured to every person in the country by law. Indian mental health legislation, as per a 2017 study, meets 68% (119/175) of the World Health Organization (WHO) standards laid down in the WHO Checklist of Mental Health Legislation. However, human resources and expertise in the field of mental health in India is significantly low when compared to the population of the country. The allocation of the national healthcare budget to mental health is also low, standing at 0.16%. India's mental health policy was released in 2014.
References
- ↑ "National health policy: a draft prepared by the Indian Medical Association". Journal of the Indian Medical Association. 72 (6): 144–7. 16 March 1979. PMID 512387.
- ↑ Chokshi, M; Patil, B; Khanna, R; Neogi, SB; Sharma, J; Paul, VK; Zodpey, S (December 2016). "Health systems in India". Journal of Perinatology. 36 (s3): S9–S12. doi:10.1038/jp.2016.184. PMC 5144115 . PMID 27924110.
- ↑ Kothia, NR; Bommireddy, VS; Devaki, T; Vinnakota, NR; Ravoori, S; Sanikommu, S; Pachava, S (26 July 2015). "Assessment of the Status of National Oral Health Policy in India". International Journal of Health Policy and Management. 4 (9): 575–81. doi:10.15171/ijhpm.2015.137. PMC 4556573 . PMID 26340486.
- ↑ Lahariya, C (15 June 2018). "'Ayushman Bharat' Program and Universal Health Coverage in India". Indian Pediatrics. 55 (6): 495–506. doi:10.1007/s13312-018-1341-1. PMID 29978817. S2CID 49706719.