Related Research Articles
The Centers for Disease Control and Prevention (CDC) is the national public health agency of the United States. It is a United States federal agency under the Department of Health and Human Services, and is headquartered in Atlanta, Georgia.

Botulism is a rare and potentially fatal illness caused by botulinum toxin, which is produced by the bacterium Clostridium botulinum. The disease begins with weakness, blurred vision, feeling tired, and trouble speaking. This may then be followed by weakness of the arms, chest muscles, and legs. Vomiting, swelling of the abdomen, and diarrhea may also occur. The disease does not usually affect consciousness or cause a fever.

Norovirus, also known as Norwalk virus and sometimes referred to as the winter vomiting disease, is the most common cause of gastroenteritis. Infection is characterized by non-bloody diarrhea, vomiting, and stomach pain. Fever or headaches may also occur. Symptoms usually develop 12 to 48 hours after being exposed, and recovery typically occurs within one to three days. Complications are uncommon, but may include dehydration, especially in the young, the old, and those with other health problems.

In epidemiology, an outbreak is a sudden increase in occurrences of a disease when cases are in excess of normal expectancy for the location or season. It may affect a small and localized group or impact upon thousands of people across an entire continent. The number of cases varies according to the disease-causing agent, and the size and type of previous and existing exposure to the agent. Outbreaks include many epidemics, which term is normally only for infectious diseases, as well as diseases with an environmental origin, such as a water or foodborne disease. They may affect a region in a country or a group of countries. Pandemics are near-global disease outbreaks when multiple and various countries around the Earth are soon infected.
The Council of State and Territorial Epidemiologists (CSTE) is a 501(c)(6) non-profit organization originally organized in 1955, founded in 1992, and based in Atlanta, Georgia. CSTE works to advance public health policy and workforce capacity for applied public health epidemiologists in all localities, states, and territories in the United States.
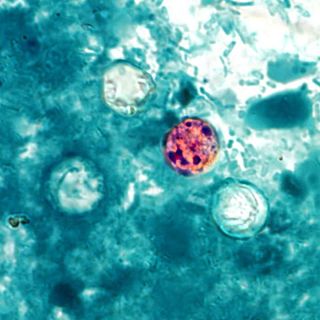
Cyclosporiasis is a disease caused by infection with Cyclospora cayetanensis, a pathogenic apicomplexan protozoan transmitted by feces or feces-contaminated food and water. Outbreaks have been reported due to contaminated fruits and vegetables. It is not spread from person to person, but can be a hazard for travelers as a cause of diarrhea.
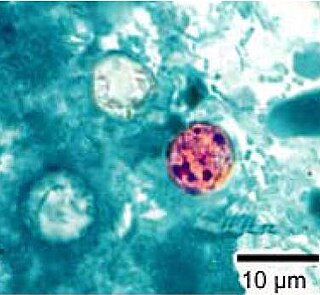
Cyclospora cayetanensis is a coccidian parasite that causes a diarrheal disease called cyclosporiasis in humans and possibly in other primates. Originally reported as a novel pathogen of probable coccidian nature in the 1980s and described in the early 1990s, it was virtually unknown in developed countries until awareness increased due to several outbreaks linked with fecally contaminated imported produce. C. cayetanensis has since emerged as an endemic cause of diarrheal disease in tropical countries and a cause of traveler's diarrhea and food-borne infections in developed nations. This species was placed in the genus Cyclospora because of the spherical shape of its sporocysts. The specific name refers to the Cayetano Heredia University in Lima, Peru, where early epidemiological and taxonomic work was done.

Waterborne diseases are conditions caused by pathogenic micro-organisms that are transmitted by water. These diseases can be spread while bathing, washing, drinking water, or by eating food exposed to contaminated water. They are a pressing issue in rural areas amongst developing countries all over the world. While diarrhea and vomiting are the most commonly reported symptoms of waterborne illness, other symptoms can include skin, ear, respiratory, or eye problems. Lack of clean water supply, sanitation and hygiene (WASH) are major causes for the spread of waterborne diseases in a community. Therefore, reliable access to clean drinking water and sanitation is the main method to prevent waterborne diseases.
Public health informatics has been defined as the systematic application of information and computer science and technology to public health practice, research, and learning. It is one of the subdomains of health informatics, data management applied to medical systems.

Disease surveillance is an epidemiological practice by which the spread of disease is monitored in order to establish patterns of progression. The main role of disease surveillance is to predict, observe, and minimize the harm caused by outbreak, epidemic, and pandemic situations, as well as increase knowledge about which factors contribute to such circumstances. A key part of modern disease surveillance is the practice of disease case reporting.
A notifiable disease is any disease that is required by law to be reported to government authorities. The collation of information allows the authorities to monitor the disease, and provides early warning of possible outbreaks. In the case of livestock diseases, there may also be the legal requirement to kill the infected livestock upon notification. Many governments have enacted regulations for reporting of both human and animal diseases.
The Association of Public Health Laboratories (APHL) is a membership organization in the United States representing the laboratories that protect the health and safety of the public. APHL serves as a liaison between public health laboratories and federal and international agencies. Membership consists of local, state, county, and territorial public health laboratories; public health environmental, agricultural and veterinary laboratories; and corporations and individuals with an interest in public health and laboratory science. APHL is a non-profit, 501(c)(3) organization with a history of over fifty years.
The Centers for Disease Control and Prevention (CDC), formed in 1946, is the leading national public health institute of the United States. It is a United States federal agency, under the United States Department of Health and Human Services. Its main goal is to protect public health and safety through the control and prevention of disease, injury, and disability in the US and internationally.

Alexander Duncan Langmuir was an American epidemiologist who served as Chief Epidemiologist of the Centers for Disease Control and Prevention (CDC) from 1949 to 1970, developing the Epidemic Intelligence Service (EIS) as a training program for epidemiologists.
BioSense is a program of the Centers for Disease Control and Prevention (CDC) that tracks health problems as they evolve and provides public health officials with the data, information and tools they need to understand developing health events. The system uses reports from local hospitals to conduct syndromic surveillance and identify trends in disease. The system began development in 2003. Its intended purpose was as an integrated nationwide health surveillance system to catch disease outbreaks and bioterrorism events such as the anthrax scare were key motivations for its development. It has faced criticism from congress and local health authorities over its cost and utility. Moreover, early versions of the system lacked uptake in part due to reluctance of hospital leaders to provide information directly to the government. Regardless, these systems have proved useful in monitoring the health effects of natural disasters, widespread outbreaks and monitoring epidemiological data on a national scale. More recently the system has also been used to monitor the effects of lifestyle such as vaping induced acute lung injuries.
The Waterborne Disease and Outbreak Surveillance System (WBDOSS) is a national surveillance system maintained by the U.S. Centers for Disease Control and Prevention (CDC). The WBDOSS receives data about waterborne disease outbreaks and single cases of waterborne diseases of public health importance in the United States and then disseminates information about these diseases, outbreaks, and their causes. WBDOSS was initiated in 1971 by CDC, the Council of State and Territorial Epidemiologists (CSTE), and the Environmental Protection Agency (EPA). Data are reported by public health departments in individual states, territories, and the Freely Associated States. Although initially designed to collect data about drinking water outbreaks in the United States, WBDOSS now includes outbreaks associated with recreational water, as well as outbreaks associated with water that is not intended for drinking (non-recreational) and water for which the intended use is unknown.

An outbreak of human monkeypox began in May 2003 in the United States. By July, a total of 71 cases were found in six Midwestern states including Wisconsin, Indiana (16), Illinois (12), Kansas (1), Missouri (2), and Ohio (1). The cause of the outbreak was traced to three species of African rodents imported from Ghana on April 9, 2003, into the United States by an exotic animal importer in Texas. These were shipped from Texas to an Illinois distributor, who housed them with prairie dogs, which then became infected.
Occupational epidemiology is a subdiscipline of epidemiology that focuses on investigations of workers and the workplace. Occupational epidemiologic studies examine health outcomes among workers, and their potential association with conditions in the workplace including noise, chemicals, heat, or radiation, or work organization such as schedules.

Matthew L. Boulton is an American epidemiologist and physician. He currently serves as the Editor-in-Chief of the American Journal of Preventive Medicine, and is the former Chief Medical Executive, State Epidemiologist, and Director of the Bureau of Epidemiology for the State of Michigan. At the University of Michigan School of Public Health, Boulton is Senior Associate Dean for Global Public Health, the Pearl L. Kendrick Collegiate Professor of Global Health, and a Professor of Epidemiology, Professor of Preventive Medicine, and a Professor of Internal Medicine, Infectious Disease Division, at Michigan Medicine.

Outbreak response or outbreak control measures are acts which attempt to minimize the spread of or effects of a disease outbreak. Outbreak response includes aspects of general disease control such as maintaining adequate hygiene, but may also include responses that extend beyond traditional healthcare settings and are unique to an outbreak, such as physical distancing, contact tracing, mapping of disease clusters, or quarantine. Some measures such as isolation are also useful in preventing an outbreak from occurring in the first place.
References
- 1 2 CDC (2024-09-17). "About the National Outbreak Reporting System (NORS)". National Outbreak Reporting System (NORS). Retrieved 2024-12-01.
- ↑ Lynch M, Painter J, Woodruff R, et al. Surveillance for Foodborne-Disease Outbreaks --- United States, 1998—2002 In: Surveillance Summaries, November 10, 2006. MMWR; 55(SS10);1-34
- ↑ Yoder J, Hlavsa M, Craun GF, et al. Surveillance for waterborne disease and outbreaks associated with recreational water use and other aquatic facility –associated health events—United States, 2005-2006. In: Surveillance Summaries, September 12, 2008. MMWR; 57(No. SS-9): 1-38
- ↑ Yoder J, Roberts V, Craun, GF, et al. Surveillance for waterborne disease and outbreaks associated with drinking water and water not intended for drinking—United States, 2005-2006. In: Surveillance Summaries, September 12, 2008. MMWR; 57(No. SS-9): 39-69.
- ↑ CDC (2024-09-11). "Reporting Guidance and Training". National Outbreak Reporting System (NORS). Retrieved 2024-12-01.