Related Research Articles

Cytopathology is a branch of pathology that studies and diagnoses diseases on the cellular level. The discipline was founded by George Nicolas Papanicolaou in 1928. Cytopathology is generally used on samples of free cells or tissue fragments, in contrast to histopathology, which studies whole tissues. Cytopathology is frequently, less precisely, called "cytology", which means "the study of cells".

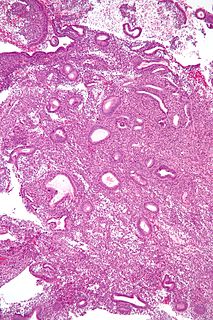
A biopsy is a medical test commonly performed by a surgeon, interventional radiologist, or an interventional cardiologist. The process involves extraction of sample cells or tissues for examination to determine the presence or extent of a disease. The tissue is then fixed, dehydrated, embedded, sectioned, stained and mounted before it is generally examined under a microscope by a pathologist; it may also be analyzed chemically. When an entire lump or suspicious area is removed, the procedure is called an excisional biopsy. An incisional biopsy or core biopsy samples a portion of the abnormal tissue without attempting to remove the entire lesion or tumor. When a sample of tissue or fluid is removed with a needle in such a way that cells are removed without preserving the histological architecture of the tissue cells, the procedure is called a needle aspiration biopsy. Biopsies are most commonly performed for insight into possible cancerous or inflammatory conditions.

Virtual colonoscopy is the use of CT scanning or magnetic resonance imaging (MRI) to produce two- and three-dimensional images of the colon, from the lowest part, the rectum, to the lower end of the small intestine, and to display the images on an electronic display device. The procedure is used to screen for colon cancer and polyps, and may detect diverticulosis. A virtual colonoscopy can provide 3D reconstructed endoluminal views of the bowel. VC provides a secondary benefit of revealing diseases or abnormalities outside the colon.
Lymph node biopsy is a test in which a lymph node or a piece of a lymph node is removed for examination under a microscope.

Fine-needle aspiration (FNA) is a diagnostic procedure used to investigate lumps or masses. In this technique, a thin, hollow needle is inserted into the mass for sampling of cells that, after being stained, are examined under a microscope (biopsy). The sampling and biopsy considered together are called fine-needle aspiration biopsy (FNAB) or fine-needle aspiration cytology (FNAC). Fine-needle aspiration biopsies are very safe minor surgical procedures. Often, a major surgical biopsy can be avoided by performing a needle aspiration biopsy instead, eliminating the need for hospitalization. In 1981, the first fine-needle aspiration biopsy in the United States was done at Maimonides Medical Center. Today, this procedure is widely used in the diagnosis of cancer and inflammatory conditions.

Prostate biopsy is a procedure in which small hollow needle-core samples are removed from a man's prostate gland to be examined for the presence of prostate cancer. It is typically performed when the result from a PSA blood test is high. It may also be considered advisable after a digital rectal exam (DRE) finds possible abnormality. PSA screening is controversial as PSA may become elevated due to non-cancerous conditions such as benign prostatic hyperplasia (BPH), by infection, or by manipulation of the prostate during surgery or catheterization. Additionally many prostate cancers detected by screening develop so slowly that they would not cause problems during a man's lifetime, making the complications due to treatment unnecessary.
Transurethral needle ablation is a technique that uses low energy radio frequency delivered through two needles to ablate excess prostate tissue. A cystoscope/catheter deploys the needles toward the obstructing prostate tissue is inserted into the urethra directly through the penis under local anesthetic before the procedure begins. The energy from the probe heats the abnormal prostate tissue without damaging the urethra. The resulting scar tissue later atrophies, reducing the size of the prostate which in turn reduces the constriction of the urethra. It can be done with a local anesthetic on an outpatient basis. It takes about an hour to perform the procedure. It takes about 30 days for the ablated prostate tissue to resorb.

Surgical pathology is the most significant and time-consuming area of practice for most anatomical pathologists. Surgical pathology involves gross and microscopic examination of surgical specimens, as well as biopsies submitted by surgeons and non-surgeons such as general internists, medical subspecialists, dermatologists, and interventional radiologists.
The endometrial biopsy is a medical procedure that involves taking a tissue sample of the lining of the uterus. The tissue subsequently undergoes a histologic evaluation which aids the physician in forming a diagnosis.
Stereotactic biopsy, also known as stereotactic core biopsy, is a biopsy procedure that uses a computer and imaging performed in at least two planes to localize a target lesion in three-dimensional space and guide the removal of tissue for examination by a pathologist under a microscope. Stereotactic core biopsy makes use of the underlying principle of parallax to determine the depth or "Z-dimension" of the target lesion.
Malignant pleural effusion is a condition in which cancer causes an abnormal amount of fluid to collect between the thin layers of tissue (pleura) lining the outside of the lung and the wall of the chest cavity. Lung cancer and breast cancer account for about 50-65% of malignant pleural effusions. Other common causes include pleural mesothelioma and lymphoma.

A Mammotome device is a vacuum-assisted breast biopsy (VAC) device that uses image guidance such as x-ray, ultrasound and/or MRI to perform breast biopsies. A biopsy using a Mammotome device can be done on an outpatient basis with a local anesthetic.
Transperineal biopsy is a biopsy procedure in which a sample of tissue is removed from the prostate for examination under a microscope. The sample is removed with a thin needle that is inserted through the skin of the perineum and into the prostate. Magnetic Resonance Imaging (MRI-Guided) is a technique used to perform prostate biopsy.
Transrectal biopsy is a biopsy procedure in which a sample of tissue is removed from the prostate using a thin needle that is inserted through the rectum and into the prostate. Transrectal ultrasound (TRUS) is usually used to guide the needle. The sample is examined under a microscope to see if it contains cancer.

Salivary gland tumours also known as mucous gland adenomas or neoplasms are tumours that form in the tissues of salivary glands. The salivary glands are classified as major or minor. The major salivary glands consist of the parotid, submandibular, and sublingual glands. The minor salivary glands consist of 800-1000 small mucus-secreting glands located throughout the lining of the oral cavity. Patients with these types of tumours may be asymptomatic.
Comedocarcinoma is a kind of breast cancer that demonstrates comedonecrosis, which is the central necrosis of cancer cells within involved ducts. Comedocarcinomas are usually non-infiltrating and intraductal tumors, characterized as a comedo-type, high-grade ductal carcinoma in situ (DCIS). However, there have been accounts of comedocarcinoma which has then diversified into other cell types and developed into infiltrating (invasive) ductal carcinoma. Recurrence and survival rates differ for invasive breast cancer which has originated as comedocarcinoma compared with other types of cancer cells.

High-grade prostatic intraepithelial neoplasia (HGPIN) is an abnormality of prostatic glands and believed to precede the development of prostate adenocarcinoma.
FNA mapping is an application of fine-needle aspiration (FNA) to the testis for the diagnosis of male infertility. FNA cytology has been used to examine pathological human tissue from various organs for over 100 years. As an alternative to open testicular biopsy for the last 40 years, FNA mapping has helped to characterize states of human male infertility due to defective spermatogenesis. Although recognized as a reliable, and informative technique, testis FNA has not been widely used in U.S. to evaluate male infertility. Recently, however, testicular FNA has gained popularity as both a diagnostic and therapeutic tool for the management of clinical male infertility for several reasons:
- The testis is an ideal organ for evaluation by FNA because of its uniform cellularity and easy accessibility.
- The trend toward minimally invasive procedures and cost-containment views FNA favorably compared to surgical testis biopsy.
- The realization that the specific histologic abnormality observed on testis biopsy has no definite correlation to either the etiology of infertility or to the ability to find sperm for assisted reproduction.
- Assisted reproduction has undergone dramatic advances such that testis sperm are routinely used for biological pregnancies, thus fueling the development of novel FNA techniques to both locate and procure sperm.

A breast mass, also known as a breast lump, is a localized swelling that feel different from the surrounding tissue. Breast pain, nipple discharge, or skin changes may be present. Concerning findings include masses that are hard, do not move easily, are of an irregular shape, or are firmly attached to surrounding tissue.

A breast biopsy is usually done after a suspicious lesion is discovered on either mammography or ultrasound to get tissue for pathological diagnosis. Several methods for a breast biopsy now exist. The most appropriate method of biopsy for a patient depends upon a variety of factors, including the size, location, appearance and characteristics of the abnormality. The different types of breast biopsies include fine-needle aspiration (FNA), vacuum-assisted biopsy, core needle biopsy, and surgical excision biopsy. Breast biopsies can be done under ultrasound, MRI or a stereotactic biopsy technique. Vacuum assisted biopsies are typically done using stereotactic techniques when the suspicious lesion can only be seen on mammography. On average, 5-10 biopsies of a suspicious breast lesion will lead to the diagnosis of one case of breast cancer.
References
- Needle-localized biopsy entry in the public domain NCI Dictionary of Cancer Terms
![]() This article incorporates public domain material from the U.S. National Cancer Institute document: "Dictionary of Cancer Terms".
This article incorporates public domain material from the U.S. National Cancer Institute document: "Dictionary of Cancer Terms".