Pathology is the study of disease. The word pathology also refers to the study of disease in general, incorporating a wide range of biology research fields and medical practices. However, when used in the context of modern medical treatment, the term is often used in a narrower fashion to refer to processes and tests that fall within the contemporary medical field of "general pathology", an area that includes a number of distinct but inter-related medical specialties that diagnose disease, mostly through analysis of tissue and human cell samples. Idiomatically, "a pathology" may also refer to the predicted or actual progression of particular diseases. The suffix pathy is sometimes used to indicate a state of disease in cases of both physical ailment and psychological conditions. A physician practicing pathology is called a pathologist.

Cytopathology is a branch of pathology that studies and diagnoses diseases on the cellular level. The discipline was founded by George Nicolas Papanicolaou in 1928. Cytopathology is generally used on samples of free cells or tissue fragments, in contrast to histopathology, which studies whole tissues. Cytopathology is frequently, less precisely, called "cytology", which means "the study of cells".

Cutaneous squamous-cell carcinoma (cSCC), also known as squamous-cell carcinoma of the skin or squamous-cell skin cancer, is one of the three principal types of skin cancer, alongside basal-cell carcinoma and melanoma. cSCC typically presents as a hard lump with a scaly surface, though it may also present as an ulcer. Onset and development often occurs over several months.

Oral cancer, also known as oral cavity cancer, tongue cancer or mouth cancer, is a cancer of the lining of the lips, mouth, or upper throat. In the mouth, it most commonly starts as a painless red or white patch, that thickens, gets ulcerated and continues to grow. When on the lips, it commonly looks like a persistent crusting ulcer that does not heal, and slowly grows. Other symptoms may include difficult or painful swallowing, new lumps or bumps in the neck, a swelling in the mouth, or a feeling of numbness in the mouth or lips.

Malignancy is the tendency of a medical condition to become progressively worse; the term is most familiar as a characterization of cancer.

Melanoma is the most dangerous type of skin cancer; it develops from the melanin-producing cells known as melanocytes. It typically occurs in the skin, but may rarely occur in the mouth, intestines, or eye.
A thymoma is a tumor originating from the epithelial cells of the thymus that is considered a rare neoplasm. Thymomas are frequently associated with neuromuscular disorders such as myasthenia gravis; thymoma is found in 20% of patients with myasthenia gravis. Once diagnosed, thymomas may be removed surgically. In the rare case of a malignant tumor, chemotherapy may be used.

Head and neck cancer is a general term encompassing multiple cancers that can develop in the head and neck region. These include cancers of the mouth, tongue, gums and lips, voice box (laryngeal), throat, salivary glands, nose and sinuses.

Fibroadenomas are benign breast tumours characterized by an admixture of stromal and epithelial tissue. Breasts are made of lobules and ducts. These are surrounded by glandular, fibrous and fatty tissues. Fibroadenomas develop from the lobules. The glandular tissue and ducts grow over the lobule to form a solid lump.

Fine-needle aspiration (FNA) is a diagnostic procedure used to investigate lumps or masses. In this technique, a thin, hollow needle is inserted into the mass for sampling of cells that, after being stained, are examined under a microscope (biopsy). The sampling and biopsy considered together are called fine-needle aspiration biopsy (FNAB) or fine-needle aspiration cytology (FNAC). Fine-needle aspiration biopsies are very safe for minor surgical procedures. Often, a major surgical biopsy can be avoided by performing a needle aspiration biopsy instead, eliminating the need for hospitalization. In 1981, the first fine-needle aspiration biopsy in the United States was done at Maimonides Medical Center. The modern procedure is widely used to diagnose cancer and inflammatory conditions. Fine needle aspiration is generally considered a safe procedure. Complications are infrequent.

Invasive carcinoma of no special type, invasive breast carcinoma of no special type (IBC-NST), invasive ductal carcinoma (IDC), infiltrating ductal carcinoma (IDC) or invasive ductal carcinoma, not otherwise specified (NOS) is a disease. For international audiences this article will use "invasive carcinoma NST" because it is the preferred term of the World Health Organization (WHO).

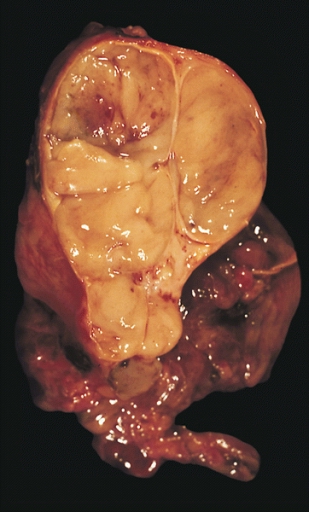
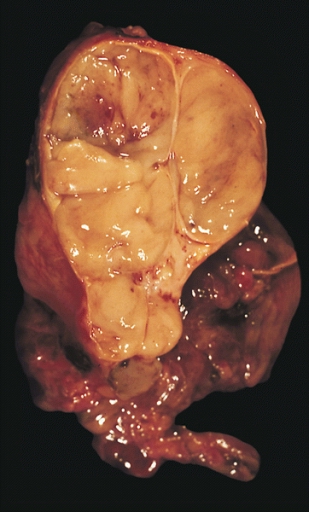
Phyllodes tumors, are a rare type of biphasic fibroepithelial mass that form from the periductal stromal and epithelial cells of the breast. They account for less than 1% of all breast neoplasms. They were previously termed cystosarcoma phyllodes, coined by Johannes Müller in 1838, before being renamed to phyllodes tumor by the World Health Organization in 2003. Phullon, which means 'leaf' in Greek, describes the unique papillary projections characteristic of phyllodes tumors on histology. Diagnosis is made via a core-needle biopsy and treatment is typically surgical resection with wide margins (>1 cm), due to their propensity to recur.

Cervical intraepithelial neoplasia (CIN), also known as cervical dysplasia, is the abnormal growth of cells on the surface of the cervix that could potentially lead to cervical cancer. More specifically, CIN refers to the potentially precancerous transformation of cells of the cervix.

Surgical pathology is the most significant and time-consuming area of practice for most anatomical pathologists. Surgical pathology involves gross and microscopic examination of surgical specimens, as well as biopsies submitted by surgeons and non-surgeons such as general internists, medical subspecialists, dermatologists, and interventional radiologists.

Skin biopsy is a biopsy technique in which a skin lesion is removed to be sent to a pathologist to render a microscopic diagnosis. It is usually done under local anesthetic in a physician's office, and results are often available in 4 to 10 days. It is commonly performed by dermatologists. Skin biopsies are also done by family physicians, internists, surgeons, and other specialties. However, performed incorrectly, and without appropriate clinical information, a pathologist's interpretation of a skin biopsy can be severely limited, and therefore doctors and patients may forgo traditional biopsy techniques and instead choose Mohs surgery.

A circulating tumor cell (CTC) is a cancer cell from a primary tumor that has shed into the blood of the circulatory system, or the lymph of the lymphatic system. CTCs are carried around the body to other organs where they may leave the circulation and become the seeds for the subsequent growth of secondary tumors. This is known as metastasis, responsible for most cancer-related deaths.

A breast biopsy is usually done after a suspicious lesion is discovered on either mammography or ultrasound to get tissue for pathological diagnosis. Several methods for a breast biopsy now exist. The most appropriate method of biopsy for a patient depends upon a variety of factors, including the size, location, appearance and characteristics of the abnormality. The different types of breast biopsies include fine-needle aspiration (FNA), vacuum-assisted biopsy, core needle biopsy, and surgical excision biopsy. Breast biopsies can be done utilizing ultrasound, MRI or a stereotactic biopsy imaging guidance. Vacuum assisted biopsies are typically done using stereotactic techniques when the suspicious lesion can only be seen on mammography. On average, 5–10 biopsies of a suspicious breast lesion will lead to the diagnosis of one case of breast cancer. Needle biopsies have largely replaced open surgical biopsies in the initial assessment of imaging as well as palpable abnormalities in the breast.
A liquid biopsy, also known as fluid biopsy or fluid phase biopsy, is the sampling and analysis of non-solid biological tissue, primarily blood. Like traditional biopsy, this type of technique is mainly used as a diagnostic and monitoring tool for diseases such as cancer, with the added benefit of being largely non-invasive. Liquid biopsies may also be used to validate the efficiency of a cancer treatment drug by taking multiple samples in the span of a few weeks. The technology may also prove beneficial for patients after treatment to monitor relapse.
CAPP-Seq is a next-generation sequencing based method used to quantify circulating DNA in cancer (ctDNA). The method was introduced in 2014 by Ash Alizadeh and Maximilian Diehn’s laboratories at Stanford, as a tool for measuring Cell-free tumor DNA which is released from dead tumor cells into the blood and thus may reflect the entire tumor genome. This method can be generalized for any cancer type that is known to have recurrent mutations. CAPP-Seq can detect one molecule of mutant DNA in 10,000 molecules of healthy DNA. The original method was further refined in 2016 for ultra sensitive detection through integration of multiple error suppression strategies, termed integrated Digital Error Suppression (iDES). The use of ctDNA in this technique should not be confused with circulating tumor cells (CTCs); these are two different entities.
Urinary cell-free DNA (ucfDNA) refers to DNA fragments in urine released by urogenital and non-urogenital cells. Shed cells on urogenital tract release high- or low-molecular-weight DNA fragments via apoptosis and necrosis, while circulating cell-free DNA (cfDNA) that passes through glomerular pores contributes to low-molecular-weight DNA. Most of the ucfDNA is low-molecular-weight DNA in the size of 150-250 base pairs. The detection of ucfDNA composition allows the quantification of cfDNA, circulating tumour DNA, and cell-free fetal DNA components. Many commercial kits and devices have been developed for ucfDNA isolation, quantification, and quality assessment.