Related Research Articles
Body substance isolation is a practice of isolating all body substances of individuals undergoing medical treatment, particularly emergency medical treatment of those who might be infected with illnesses such as HIV, or hepatitis so as to reduce as much as possible the chances of transmitting these illnesses. BSI is similar in nature to universal precautions, but goes further in isolating workers from pathogens, including substances now known to carry HIV.

Universal precautions refers to the practice, in medicine, of avoiding contact with patients' bodily fluids, by means of the wearing of nonporous articles such as medical gloves, goggles, and face shields. The infection control techniques were essentially good hygiene habits, such as hand washing and the use of gloves and other barriers, the correct handling of hypodermic needles, scalpels, and aseptic techniques. Following the AIDS outbreak in the 1980s, the US CDC formally introduced them in 1985–88. Every patient was treated as if infected, and therefore precautions were taken to minimize risk.

Hepatitis is inflammation of the liver tissue. Some people or animals with hepatitis have no symptoms, whereas others develop yellow discoloration of the skin and whites of the eyes (jaundice), poor appetite, vomiting, tiredness, abdominal pain, and diarrhea. Hepatitis is acute if it resolves within six months, and chronic if it lasts longer than six months. Acute hepatitis can resolve on its own, progress to chronic hepatitis, or (rarely) result in acute liver failure. Chronic hepatitis may progress to scarring of the liver (cirrhosis), liver failure, and liver cancer.

A blood-borne disease is a disease that can be spread through contamination by blood and other body fluids. Blood can contain pathogens of various types, chief among which are microorganisms, like bacteria and parasites, and non-living infectious agents such as viruses. Three blood-borne pathogens in particular, all viruses, are cited as of primary concern to health workers by the CDC-NIOSH: HIV, hepatitis B (HVB), & hepatitis C (HVC).
Needle sharing is the practice of intravenous drug-users by which a needle or syringe is shared by multiple individuals to administer intravenous drugs such as heroin, steroids, and hormones. This is a primary vector for blood-borne diseases which can be transmitted through blood. People who inject drugs (PWID) are at an increased risk for Hepatitis C (HCV) and HIV due to needle sharing practices. From 1933 to 1943, malaria was spread between users in the New York City area by this method. Afterwards, the use of quinine as a cutting agent in drug mixes became more common. Harm reduction efforts including safe disposal of needles, supervised injection sites, and public education may help bring awareness on safer needle sharing practices.

An injection is the act of administering a liquid, especially a drug, into a person's body using a needle and a syringe. An injection is considered a form of parenteral drug administration; it does not involve absorption in the digestive tract. This allows the medication to be absorbed more rapidly and avoid the first pass effect. There are many types of injection, which are generally named after the body tissue the injection is administered into. This includes common injections such as subcutaneous, intramuscular, and intravenous injections, as well as less common injections such as intraperitoneal, intraosseous, intracardiac, intraarticular, and intracavernous injections.
Post-exposure prophylaxis, also known as post-exposure prevention (PEP), is any preventive medical treatment started after exposure to a pathogen in order to prevent the infection from occurring.

Tropical medicine is an interdisciplinary branch of medicine that deals with health issues that occur uniquely, are more widespread, or are more difficult to control in tropical and subtropical regions.

A needlestick injury is the penetration of the skin by a hypodermic needle or other sharp object that has been in contact with blood, tissue or other body fluids before the exposure. Even though the acute physiological effects of a needlestick injury are generally negligible, these injuries can lead to transmission of blood-borne diseases, placing those exposed at increased risk of infection from disease-causing pathogens, such as the hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV). Among healthcare workers and laboratory personnel worldwide, more than 25 blood-borne virus infections have been reported to have been caused by needlestick injuries. In addition to needlestick injuries, transmission of these viruses can also occur as a result of contamination of the mucous membranes, such as those of the eyes, with blood or body fluids, but needlestick injuries make up more than 80% of all percutaneous exposure incidents in the United States. Various other occupations are also at increased risk of needlestick injury, including law enforcement, laborers, tattoo artists, food preparers, and agricultural workers.
Infection prevention & control is the discipline concerned with preventing healthcare-associated infections; a practical rather than academic sub-discipline of epidemiology. In Northern Europe, infection prevention and control is expanded from healthcare into a component in public health, known as "infection protection". It is an essential part of the infrastructure of health care. Infection control and hospital epidemiology are akin to public health practice, practiced within the confines of a particular health-care delivery system rather than directed at society as a whole.

A needle remover is a device used to physically remove a needle from a syringe. In developing countries, there is still a need for improvements in needle safety in hospital settings as most of the needle removal processes are done manually and under severe risk of hazard from needles puncturing skin risking infection. These countries cannot afford needles with individual safety devices attached, so needle-removers must be used to remove the needle from the syringe. This lowers possible pathogen spread by preventing the reuse of the syringes, reducing incidents of accidental needle-sticks, and facilitating syringe disposal.

Sharps waste is a form of biomedical waste composed of used "sharps", which includes any device or object used to puncture or lacerate the skin. Sharps waste is classified as biohazardous waste and must be carefully handled. Common medical materials treated as sharps waste are hypodermic needles, disposable scalpels and blades, contaminated glass and certain plastics, and guidewires used in surgery.
Human Immunodeficiency Virus (HIV) and Hepatitis C Virus (HCV) co-infection is a multi-faceted, chronic condition that significantly impacts public health. According to the World Health Organization (WHO), 2 to 15% of those infected with HIV are also affected by HCV, increasing their risk of morbidity and mortality due to accelerated liver disease. The burden of co-infection is especially high in certain high-risk groups, such as intravenous drug users and men who have sex with men. These individuals who are HIV-positive are commonly co-infected with HCV due to shared routes of transmission including, but not limited to, exposure to HIV-positive blood, sexual intercourse, and passage of the Hepatitis C virus from mother to infant during childbirth.

Drug injection is a method of introducing a drug into the bloodstream via a hollow hypodermic needle, which is pierced through the skin into the body. Intravenous therapy, a form of drug injection, is universally practiced in modernized medical care. As of 2004, there were 13.2 million people worldwide who self-administered injection drugs outside of medical supervision, of which 22% are from developed countries.
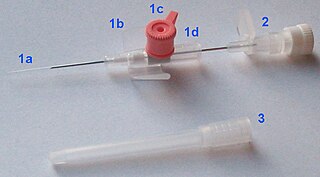
In medicine, a peripheral venous catheter, peripheral venous line, peripheral venous access catheter, or peripheral intravenous catheter, is a catheter placed into a peripheral vein for venous access to administer intravenous therapy such as medication fluids.

Sexually transmitted infections (STIs), also referred to as sexually transmitted diseases (STDs) and the older term venereal diseases, are infections that are spread by sexual activity, especially vaginal intercourse, anal sex, and oral sex. STIs often do not initially cause symptoms, which results in a risk of passing the infection on to others. Symptoms and signs of STIs may include vaginal discharge, penile discharge, ulcers on or around the genitals, and pelvic pain. Some STIs can cause infertility.
A pin prick attack is an assault on another person with a needle or syringe tainted with the blood of somebody carrying a blood-borne disease, such as HIV. Although there have been numerous cases of people being attacked with needles and syringes, the idea that people infected with AIDS have deliberately attempted to infect others in this manner is generally considered an urban legend, real cases of infection of HIV in this manner were typically taken from infected victims rather than from infected attackers.
ICU Medical, Inc. is a San Clemente, California-based company with global operations that develops, manufactures, and sells medical technologies used in vascular therapy, oncology, and critical care applications.

A safety syringe is a syringe with a built-in safety mechanism to reduce the risk of needlestick injuries to healthcare workers and others. The needle on a safety syringe can be detachable or permanently attached. On some models, a sheath is placed over the needle, whereas in others the needle retracts into the barrel. Safety needles serve the same functions as safety syringes, but the protective mechanism is a part of the needle rather than the syringe. Legislation requiring safety syringes or equivalents has been introduced in many nations since needlestick injuries and re-use prevention became the focus of governments and safety bodies.
Infectious diseases within American correctional settings are a concern within the public health sector. The corrections population is susceptible to infectious diseases through exposure to blood and other bodily fluids, drug injection, poor health care, prison overcrowding, demographics, security issues, lack of community support for rehabilitation programs, and high-risk behaviors. The spread of infectious diseases, such as HIV and other sexually transmitted diseases, hepatitis C (HCV), hepatitis B (HBV), and tuberculosis, result largely from needle-sharing, drug use, and consensual and non-consensual sex among prisoners. HIV and hepatitis C need specific attention because of the specific public health concerns and issues they raise.
References
- ↑ Curran, Evonne (September 2016). "Needleless connectors: the vascular access catheter's microbial gatekeeper". Journal of Infection Prevention. 17 (5): 234–240. doi:10.1177/1757177416657164. ISSN 1757-1774. PMC 5102078 . PMID 28989484.
- ↑ "Needlestick injury | betterhealth.vic.gov.au". www.betterhealth.vic.gov.au. Retrieved 2021-03-16.
- ↑ "Bloodborne Infectious Diseases: HIV/AIDS, Hepatitis B, Hepatitis C". Medical Management. 2013-11-19. Retrieved 2020-07-24.
- ↑ "CDC - Bloodborne Infectious Diseases - Emergency Needlestick Information - NIOSH Workplace Safety and Health Topic". www.cdc.gov. 2018-11-21. Retrieved 2021-03-16.
- ↑ "Central line infections - hospitals: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2021-03-16.
- ↑ Moureau, Nancy L.; Dawson, Robert B. (December 2010). "Needleless connector know-how". Nursing Management. 41 (12): 40–41. doi: 10.1097/01.NUMA.0000390461.26871.25 . ISSN 0744-6314. PMID 21116154.
- ↑ "Needleless connector". Patents.Google. 25 April 1996. Retrieved 1 April 2021.