Related Research Articles
In the United States, a health maintenance organization (HMO) is a medical insurance group that provides health services for a fixed annual fee. It is an organization that provides or arranges managed care for health insurance, self-funded health care benefit plans, individuals, and other entities, acting as a liaison with health care providers on a prepaid basis. The US Health Maintenance Organization Act of 1973 required employers with 25 or more employees to offer federally certified HMO options if the employer offers traditional healthcare options. Unlike traditional indemnity insurance, an HMO covers care rendered by those doctors and other professionals who have agreed by contract to treat patients in accordance with the HMO's guidelines and restrictions in exchange for a steady stream of customers. HMOs cover emergency care regardless of the health care provider's contracted status.
A health system, health care system or healthcare system is an organization of people, institutions, and resources that delivers health care services to meet the health needs of target populations.

Health care, or healthcare, is the improvement of health via the prevention, diagnosis, treatment, amelioration or cure of disease, illness, injury, and other physical and mental impairments in people. Health care is delivered by health professionals and allied health fields. Medicine, dentistry, pharmacy, midwifery, nursing, optometry, audiology, psychology, occupational therapy, physical therapy, athletic training, and other health professions all constitute health care. The term includes work done in providing primary care, secondary care, tertiary care, and public health.

The Health Insurance Portability and Accountability Act of 1996 is a United States Act of Congress enacted by the 104th United States Congress and signed into law by President Bill Clinton on August 21, 1996. It aimed to alter the transfer of healthcare information, stipulated the guidelines by which personally identifiable information maintained by the healthcare and healthcare insurance industries should be protected from fraud and theft, and addressed some limitations on healthcare insurance coverage. It generally prohibits healthcare providers and businesses called covered entities from disclosing protected information to anyone other than a patient and the patient's authorized representatives without their consent. The bill does not restrict patients from receiving information about themselves. Furthermore, it does not prohibit patients from voluntarily sharing their health information however they choose, nor does it require confidentiality where a patient discloses medical information to family members, friends or other individuals not employees of a covered entity.
Health insurance or medical insurance is a type of insurance that covers the whole or a part of the risk of a person incurring medical expenses. As with other types of insurance, risk is shared among many individuals. By estimating the overall risk of health risk and health system expenses over the risk pool, an insurer can develop a routine finance structure, such as a monthly premium or payroll tax, to provide the money to pay for the health care benefits specified in the insurance agreement. The benefit is administered by a central organization, such as a government agency, private business, or not-for-profit entity.
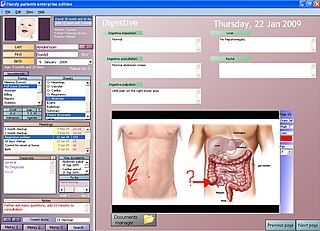
An electronic health record (EHR) is the systematized collection of patient and population electronically stored health information in a digital format. These records can be shared across different health care settings. Records are shared through network-connected, enterprise-wide information systems or other information networks and exchanges. EHRs may include a range of data, including demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal statistics like age and weight, and billing information.
The term managed care or managed healthcare is used in the United States to describe a group of activities intended to reduce the cost of providing health care and providing American health insurance while improving the quality of that care. It has become the predominant system of delivering and receiving American health care since its implementation in the early 1980s, and has been largely unaffected by the Affordable Care Act of 2010.
...intended to reduce unnecessary health care costs through a variety of mechanisms, including: economic incentives for physicians and patients to select less costly forms of care; programs for reviewing the medical necessity of specific services; increased beneficiary cost sharing; controls on inpatient admissions and lengths of stay; the establishment of cost-sharing incentives for outpatient surgery; selective contracting with health care providers; and the intensive management of high-cost health care cases. The programs may be provided in a variety of settings, such as Health Maintenance Organizations and Preferred Provider Organizations.

The right to health is the economic, social, and cultural right to a universal minimum standard of health to which all individuals are entitled. The concept of a right to health has been enumerated in international agreements which include the Universal Declaration of Human Rights, International Covenant on Economic, Social and Cultural Rights, and the Convention on the Rights of Persons with Disabilities. There is debate on the interpretation and application of the right to health due to considerations such as how health is defined, what minimum entitlements are encompassed in a right to health, and which institutions are responsible for ensuring a right to health.
A Regional Health Information Organization, also called a Health Information Exchange Organization, is a multistakeholder organization created to facilitate a health information exchange (HIE) – the transfer of healthcare information electronically across organizations – among stakeholders of that region's healthcare system. The ultimate objective is to improve the safety, quality, and efficiency of healthcare as well as access to healthcare through the efficient application of health information technology. RHIOs are also intended to support secondary use of clinical data for research as well as institution/provider quality assessment and improvement. RHIO stakeholders include smaller clinics, hospitals, medical societies, major employers and payers.
The Universal Service Fund (USF) is a system of telecommunications subsidies and fees managed by the United States Federal Communications Commission (FCC) to promote universal access to telecommunications services in the United States. The FCC established the fund in 1997 in compliance with the Telecommunications Act of 1996. Originally designed to subsidize telephone service, since 2011 the fund has expanded its goals to supporting broadband universal service. The Universal Service Fund's budget ranges from $5–8 billion per year depending on the needs of the telecommunications providers. These needs include the cost to maintain the hardware needed for their services and the services themselves. In 2022 disbursements totaled $7.4 billion, split across the USF's four main programs: $2.1 billion for the E-rate program, $4.2 billion for the high-cost program, $0.6 billion for the Lifeline program, and $0.5 billion for the rural health care program.
Case management is a managed care technique within the health care coverage system of the United States. It involves an integrated system that manages the delivery of comprehensive healthcare services for enrolled patients. Case managers are employed in almost every aspect of health care and these employ different approaches in the control of clinical actions.
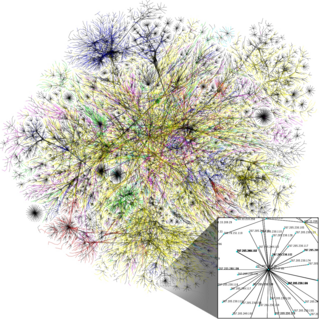
The Internet in the United States grew out of the ARPANET, a network sponsored by the Advanced Research Projects Agency of the U.S. Department of Defense during the 1960s. The Internet in the United States of America in turn provided the foundation for the worldwide Internet of today.
In the United States, health insurance helps pay for medical expenses through privately purchased insurance, social insurance, or a social welfare program funded by the government. Synonyms for this usage include "health coverage", "health care coverage", and "health benefits". In a more technical sense, the term "health insurance" is used to describe any form of insurance providing protection against the costs of medical services. This usage includes both private insurance programs and social insurance programs such as Medicare, which pools resources and spreads the financial risk associated with major medical expenses across the entire population to protect everyone, as well as social welfare programs like Medicaid and the Children's Health Insurance Program, which both provide assistance to people who cannot afford health coverage.

The Military Health System (MHS) is the internal health care system operated within the United States Department of Defense that provides health care to active duty, Reserve component and retired U.S. Military personnel and their dependents.

The Philippine Health Insurance Corporation (PhilHealth) was created in 1995 to implement universal health coverage in the Philippines. It is a tax-exempt, government-owned and controlled corporation (GOCC) of the Philippines, and is attached to the Department of Health. On August 4, 1969, Republic Act 6111 or the Philippine Medical Care Act of 1969 was signed by President Ferdinand E. Marcos which was eventually implemented in August 1971.
Balance billing, sometimes called surprise billing, is a medical bill from a healthcare provider billing a patient for the difference between the total cost of services being charged and the amount the insurance pays. It is a pervasive practice in the United States with providers who are out of network, and therefore not subject to the rates or terms of providers who are in-network. Balance billing has a variable prevalence by market and specialty.
The Health Information Technology for Economic and Clinical Health Act, abbreviated the HITECH Act, was enacted under Title XIII of the American Recovery and Reinvestment Act of 2009. Under the HITECH Act, the United States Department of Health and Human Services resolved to spend $25.9 billion to promote and expand the adoption of health information technology. The Washington Post reported the inclusion of "as much as $36.5 billion in spending to create a nationwide network of electronic health records." At the time it was enacted, it was considered "the most important piece of health care legislation to be passed in the last 20 to 30 years" and the "foundation for health care reform."

India has a multi-payer universal health care model that is paid for by a combination of public and government regulated private health insurances along with the element of almost entirely tax-funded public hospitals. The public hospital system is essentially free for all Indian residents except for small, often symbolic co-payments in some services. Economic Survey 2022-23 highlighted that the Central and State Governments’ budgeted expenditure on the health sector reached 2.1% of GDP in FY23 and 2.2% in FY22, against 1.6% in FY21. India ranks 78th and has one of the lowest healthcare spending as a percent of GDP. It also ranks 77th on the list of countries by total health expenditure per capita.
Health care analytics is the health care analysis activities that can be undertaken as a result of data collected from four areas within healthcare: (1) claims and cost data, (2) pharmaceutical and research and development (R&D) data, (3) clinical data, and (4) patient behaviors and preferences data. Health care analytics is a growing industry in many countries including the United States, where it is expected to grow to more than $31 billion by 2022. It is also increasingly important to governments and public health agencies to support health policy and meet public expectations for transparency, as accelerated by the Covid-19 pandemic.
Ghost network refers to a form of healthcare insurance fraud where providers are listed as in a health insurance plan, but are unable to provide care. These ghost providers may no longer be eligible to practice, may have retired, may no longer accept new patients, may not actually part of the network, or may not exist. The inclusion of ghost providers may be intentional to exaggerate plan availability to encourage enrollment and falsely meet healthcare network adequacy.
References
- ↑ Bradley, Katharine; Wishon, Allison; Donnelly, Alexandra; Lechner, Amanda (November 2021). "Network Adequacy for Behavioral Health: Existing Standards and Considerations for Designing Standards". U.S. Department of Health and Human Services. HHSP233201500035I. Retrieved 22 September 2024.
 This article incorporates text from this source, which is in the public domain .
This article incorporates text from this source, which is in the public domain . - ↑ Rahim, Hannah (December 6, 2023). "Addressing Ghost Networks in Mental Health Care". Bill of Health. Petrie-Flom Center. Harvard Law School . Retrieved 22 September 2024.
- ↑ Pollitz, Karen (4 February 2022). "Network Adequacy Standards and Enforcement". KFF. Retrieved 22 September 2024.