Related Research Articles
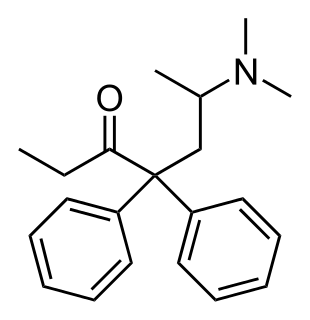
Methadone, sold under the brand names Dolophine and Methadose among others, is a synthetic opioid agonist used for chronic pain and also for opioid dependence. It is used to treat chronic pain, and it is also used to treat addiction to heroin or other opioids. Prescribed for daily use, the medicine relieves cravings and removes withdrawal symptoms. Detoxification using methadone can be accomplished in less than a month, or it may be done gradually over as long as six months. While a single dose has a rapid effect, maximum effect can take up to five days of use. The pain-relieving effects last about six hours after a single dose. After long-term use, in people with normal liver function, effects last 8 to 36 hours. Methadone is usually taken by mouth and rarely by injection into a muscle or vein.

Naloxone, sold under the brand name Narcan among others, is a medication used to reverse the effects of opioids. It is commonly used to counter decreased breathing in opioid overdose. Naloxone may also be combined with an opioid, to decrease the risk of misuse through injection. Effects begin within two minutes when given intravenously, and within five minutes when injected into a muscle. The medicine can also be administered by spraying it into a person's nose. Naloxone commonly blocks the effects of opioids for 30 to 90 minutes. Multiple doses may be required, as the duration of action of some opioids is greater than that of naloxone.

A drug overdose is the ingestion or application of a drug or other substance in quantities much greater than are recommended. Typically it is used for cases when a risk to health will potentially result. An overdose may result in a toxic state or death.

Opioids are substances that act on opioid receptors to produce morphine-like effects. Medically they are primarily used for pain relief, including anesthesia. Other medical uses include suppression of diarrhea, replacement therapy for opioid use disorder, reversing opioid overdose, and suppressing cough. Extremely potent opioids such as carfentanil are approved only for veterinary use. Opioids are also frequently used non-medically for their euphoric effects or to prevent withdrawal. Opioids can cause death and have been used for executions in the United States.

Opioid use disorder (OUD) is a substance use disorder relating to the use of an opioid. Any such disorder causes significant impairment or distress. Signs of the disorder include a strong desire to use opioids, increased tolerance to opioids, difficulty fulfilling obligations, trouble reducing use, and withdrawal symptoms with discontinuation. Opioid withdrawal symptoms may include nausea, muscle aches, diarrhea, trouble sleeping, agitation, and a low mood. Addiction and dependence are components of a substance use disorder. Complications may include opioid overdose, suicide, HIV/AIDS, hepatitis C, and problems at school, work, or home.

Buprenorphine is an opioid used to treat opioid use disorder, acute pain, and chronic pain. It can be used under the tongue (sublingual), in the cheek (buccal), by injection, as a skin patch (transdermal), or as an implant. For opioid use disorder, it is typically started when withdrawal symptoms have begun and for the first two days of treatment under direct observation of a health-care provider. In the United States, the combination formulation of buprenorphine/naloxone (Suboxone) is usually prescribed to discourage misuse by injection. Maximum pain relief is generally within an hour with effects up to 24 hours. Buprenorphine affects different types of opioid receptors in different ways. Depending on the type of receptor, it may be an agonist, partial agonist, or antagonist. In the treatment of opioid use disorder buprenorphine is an agonist/antagonist, meaning that it relieves withdrawal symptoms from other opioids and induces some euphoria, but also blocks the ability for many other opioids, including heroin, to cause an effect. Unlike full agonists like heroin or methadone, buprenorphine has a ceiling effect, such that taking more medicine will not increase the effects of the drug.

An opioid overdose is toxicity due to excessive consumption of opioids, such as morphine, codeine, heroin, fentanyl, tramadol, and methadone. This preventable pathology can be fatal if it leads to respiratory depression, a lethal condition that can cause hypoxia. Other symptoms include insufficient breathing, small pupils, and unconsciousness, however its onset can depend on the method of ingestion, the dosage and individual risk factors. Although there were over 110,000 deaths in 2017 due to opioids, individuals who survived also faced adverse complications, including permanent brain damage.

Heroin-assisted treatment (HAT), or diamorphine assisted treatment, refers to a type of Medication-Assisted Treatment (MAT) where semi-synthetic heroin is prescribed to opiate addicts who do not benefit from, or cannot tolerate, treatment with one of the established drugs used in opiate replacement therapy such as methadone or buprenorphine. For this group of patients, heroin-assisted treatment has proven superior in improving their social and health situation. It has also been shown to save money, as it significantly reduces costs incurred by trials, incarceration, health interventions and delinquency. It has also drastically reduced overdose deaths in the countries utilizing it, as patients take their dose in a controlled, professionally supervised setting, and Narcan (naloxone) is on hand in the case of an accidental overdose. Opiate related overdoses in the U.S. kill around 70,000 people per year.
In the United States, prescription monitoring programs (PMPs) or prescription drug monitoring programs (PDMPs) are state-run programs which collect and distribute data about the prescription and dispensation of federally controlled substances and, depending on state requirements, other potentially abusable prescription drugs. PMPs are meant to help prevent adverse drug-related events such as opioid overdoses, drug diversion, and substance abuse by decreasing the amount and/or frequency of opioid prescribing, and by identifying those patients who are obtaining prescriptions from multiple providers or those physicians overprescribing opioids.

Buprenorphine/naloxone, sold under the brand name Suboxone among others, is a fixed-dose combination medication that includes buprenorphine and naloxone. It is used to treat opioid use disorder, and reduces the mortality of opioid use disorder by 50%. It relieves cravings to use and withdrawal symptoms. Buprenorphine/naloxone is available for use in two different forms, under the tongue or in the cheek.
The California State Legislature passed an act to amend Section 1714.22 of the Civil Code, relating to drug overdose treatment in 2014. California Assembly Bill 1535 (2014) delegated the authority to all properly licensed California state pharmacists who had undergone a training program of at least one hour of continuing education about the pharmacology of naloxone hydrochloride to dispense naloxone under standards developed by the Medical Board of California in conjunction with the California Society of Addiction Medicine, the California Pharmacists Association, and any other appropriate entities.

The opioid epidemic is the extensive ongoing overuse of opioid medications, both from medical prescriptions and from illegal sources. The epidemic began in the United States in the late 1990s, according to the Centers for Disease Control and Prevention (CDC), when opioids were increasingly prescribed for pain management and resulted in a rise in overall opioid use throughout subsequent years. The great majority of Americans who use prescription opioids do not believe that they are misusing them.

The opioid epidemic, also referred to as the opioid crisis, is rapid increase in the overuse, misuse/abuse, and overdose deaths attributed either in part or in whole to the class of drugs opiates/opioids since the 1990s. It includes the significant medical, social, psychological, and economic consequences of the medical, non-medical, and recreational abuse of these medications.
When authorized medical personnel prescribe two or more medications together for the same condition or disease to the same patient, it is known as co-prescribing. When clinicians prescribe the opioid overdose drug naloxone to patients in conjunction with the patient's opioid prescriptions, or to patients at risk for opioid overdose, it is called a naloxone co-prescription. Due, in part, to the opioid epidemic in the United States, there are currently both a state-level and nation-wide movement in the medical and public policy fields to encourage, and sometimes require, naloxone co-prescribing. The U.S. government has issued guidelines recommending co-prescribing naloxone along with opioids. Some co-prescribing, e.g., the practice of co-prescribing benzodiazepines and certain opioid medications to patients, has been cause for concern due to the high risk of opioid overdose.
Chinazo D. Opia Cunningham is a physician, researcher, and Professor of Medicine at Albert Einstein College of Medicine in New York City. She is also the Director of Diversity Affairs for the Department of Medicine. She worked on the frontlines during the HIV/AIDS crisis in San Francisco and in 2020 began working on the frontlines of the Coronavirus disease 2019 (COVID-19) pandemic in New York City. She also specializes in treating patients with addiction, overseeing a network using buprenorphine to treat people with opioid addiction.
The New Jersey “Opioid Antidote Prescription” bill is legislation sponsored in the New Jersey State Senate. The bill, numbered NJ S. 2323, requires a co-prescription of an opioid overdose agent, such as naloxone, with prescriptions for opioid medications for patients who have a high risk of overdosing and tightens restrictions on the dispensing of opioid medications in New Jersey.
The Illinois “Opioids-Covid-19-Naloxone” Resolution is legislation sponsored in the Illinois State Senate. The bill, numbered IL SR 1184, prompts the state of Illinois to examine the rise in opioid overdoses due to the COVID-19 pandemic. The bill also urges the state to improve and increase access to naloxone, an opioid overdose reversal drug.
The South Carolina opioid overdose prevention bill is legislation sponsored in the South Carolina state legislature. The bill, numbered SC H.B. 4711 and sponsored by state Representative Russell Fry, would require prescribers to offer a prescription for naloxone to patients at high risk of an opioid overdose.
The California naloxone requirement bill is legislation passed by the California legislature and signed into law in 2018. The bill, numbered AB 2760, and sponsored by state Assembly member Jim Wood, requires medical prescribers to offer a prescription for naloxone to certain populations at higher risk of overdosing from opiate drugs.
Over a period of six months, Colorado legislation HB 20–1065, the Colorado Harm Reduction Substance Use Disorders Law, passed through both houses of the state legislature with bipartisan sponsorship and was signed into law by Governor Jared Polis (D). The law provides support mechanisms and medications to individuals with substance abuse disorder. It also provides protection to pharmacists and ordinary Good Samaritans who are attempting to assist those with the potential of drug overdose and its subsequent consequences.
References
- ↑ Scholl, Lawrence; Seth, Puja; Kariisa, Mbabazi; Wilson, Nana; Baldwin, Grant (2018-12-21). "Drug and Opioid-Involved Overdose Deaths — United States, 2013–2017". MMWR. Morbidity and Mortality Weekly Report. 67 (5152): 1419–1427. doi: 10.15585/mmwr.mm675152e1 . ISSN 0149-2195. PMC 6334822 . PMID 30605448.
- ↑ Abuse, National Institute on Drug (2020-02-20). "Opioid Overdose Reversal with Naloxone (Narcan, Evzio)". National Institute on Drug Abuse. Retrieved 2020-06-30.
- ↑ Abuse, National Institute on Drug (2020-04-03). "New York: Opioid-Involved Deaths and Related Harms". National Institute on Drug Abuse. Retrieved 2020-06-30.
- 1 2 3 https://health.ny.gov/statistics/opioid/data/pdf/nys_opioid_annual_report_2019.pdf [ bare URL PDF ]
- 1 2 https://legislation.nysenate.gov/pdf/bills/2019/S5150B [ dead link ]
- ↑ "NY State Senate Bill S5150B". NY State Senate. 2019-06-14. Retrieved 2020-06-30.
- ↑ "Senate Takes Major Steps To Combat The Opioid Crisis". NY State Senate. 2020-02-04. Retrieved 2020-06-30.