Related Research Articles

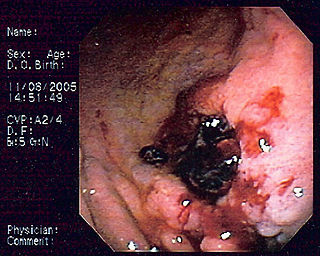
Colonoscopy or coloscopy is a medical procedure involving the endoscopic examination of the large bowel (colon) and the distal portion of the small bowel. This examination is performed using either a CCD camera or a fiber optic camera, which is mounted on a flexible tube and passed through the anus.

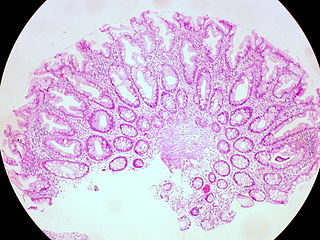
In anatomy, a polyp is an abnormal growth of tissue projecting from a mucous membrane. If it is attached to the surface by a narrow elongated stalk, it is said to be pedunculated; if it is attached without a stalk, it is said to be sessile. Polyps are commonly found in the colon, stomach, nose, ear, sinus(es), urinary bladder, and uterus. They may also occur elsewhere in the body where there are mucous membranes, including the cervix, vocal folds, and small intestine. Some polyps are tumors (neoplasms) and others are non-neoplastic, for example hyperplastic or dysplastic, which are benign. The neoplastic ones are usually benign, although some can be pre-malignant, or concurrent with a malignancy.

A precancerous condition is a condition, tumor or lesion involving abnormal cells which are associated with an increased risk of developing into cancer. Clinically, precancerous conditions encompass a variety of abnormal tissues with an increased risk of developing into cancer. Some of the most common precancerous conditions include certain colon polyps, which can progress into colon cancer, monoclonal gammopathy of undetermined significance, which can progress into multiple myeloma or myelodysplastic syndrome. and cervical dysplasia, which can progress into cervical cancer. Bronchial premalignant lesions can progress to squamous cell carcinoma of the lung.
Gastrointestinal cancer refers to malignant conditions of the gastrointestinal tract and accessory organs of digestion, including the esophagus, stomach, biliary system, pancreas, small intestine, large intestine, rectum and anus. The symptoms relate to the organ affected and can include obstruction, abnormal bleeding or other associated problems. The diagnosis often requires endoscopy, followed by biopsy of suspicious tissue. The treatment depends on the location of the tumor, as well as the type of cancer cell and whether it has invaded other tissues or spread elsewhere. These factors also determine the prognosis.

Endoscopic ultrasound (EUS) or echo-endoscopy is a medical procedure in which endoscopy is combined with ultrasound to obtain images of the internal organs in the chest, abdomen and colon. It can be used to visualize the walls of these organs, or to look at adjacent structures. Combined with Doppler imaging, nearby blood vessels can also be evaluated.
Primary gastric lymphoma is an uncommon condition, accounting for less than 15% of gastric malignancies and about 2% of all lymphomas. However, the stomach is a very common extranodal site for lymphomas. It is also the most common source of lymphomas in the gastrointestinal tract.

The submucosa is a thin layer of tissue in various organs of the gastrointestinal, respiratory, and genitourinary tracts. It is the layer of dense irregular connective tissue that supports the mucosa and joins it to the muscular layer, the bulk of overlying smooth muscle.

Colonic polypectomy is the removal of colorectal polyps in order to prevent them from turning cancerous.

A self-expandable metallic stent is a metallic tube, or stent that holds open a structure in the gastrointestinal tract to allow the passage of food, chyme, stool, or other secretions related to digestion. Surgeons insert SEMS by endoscopy, inserting a fibre optic camera—either through the mouth or colon—to reach an area of narrowing. As such, it is termed an endoprosthesis. SEMS can also be inserted using fluoroscopy where the surgeon uses an X-ray image to guide insertion, or as an adjunct to endoscopy.

An endoclip is a metallic mechanical device used in endoscopy in order to close two mucosal surfaces without the need for surgery and suturing. Its function is similar to a suture in gross surgical applications, as it is used to join together two disjointed surfaces, but, can be applied through the channel of an endoscope under direct visualization. Endoclips have found use in treating gastrointestinal bleeding, in preventing bleeding after therapeutic procedures such as polypectomy, and in closing gastrointestinal perforations. Many forms of endoclips exist of different shapes and sizes, including two and three prong devices, which can be administered using single use and reloadable systems, and may or may not open and close to facilitate placement.

A colorectal polyp is a polyp occurring on the lining of the colon or rectum. Untreated colorectal polyps can develop into colorectal cancer.

An inflammatory fibroid polyp(IFP) is an uncommon digestive system tumor. J. Vanek initially identified it as a separate pathological entity in 1949 when he reported six case reports of eosinophilic infiltration in gastric submucosal granulomas. It is a single, non-encapsulated polypoid lesion that is typically submucosal. It is characterized by a large number of small blood vessels, oedematous connective tissue, and an inflammatory eosinophilic infiltrate.
Endoscopic mucosal resection is a technique used to remove cancerous or other abnormal lesions found in the digestive tract. It is one method of performing a mucosectomy.
Solitary rectal ulcer syndrome or SRUS is a chronic, benign disorder of the rectal mucosa. It commonly occurs with varying degrees of rectal prolapse. The condition is thought to be caused by different factors, such as long term constipation, straining during defecation, and dyssynergic defecation. Treatment is by normalization of bowel habits, biofeedback, and other conservative measures. In more severe cases various surgical procedures may be indicated. The condition is relatively rare, affecting approximately 1 in 100,000 people per year. It affects mainly adults aged 30–50. Females are affected slightly more often than males. The disorder can be confused clinically with rectal cancer or other conditions such as inflammatory bowel disease, even when a biopsy is done.

The colorectal adenoma is a benign glandular tumor of the colon and the rectum. It is a precursor lesion of the colorectal adenocarcinoma. They often manifest as colorectal polyps.
Gastrointestinal intraepithelial neoplasia is also known as gastrointestinal dysplasia. Gastrointestinal dysplasia refers to abnormal growth of the epithelial tissue lining the gastrointestinal tract including the esophagus, stomach, and colon. Pancreatic, biliary, and rectal Intraepithelial Neoplasia are discussed separately. The regions of abnormal growth are confined by the basement membrane adjacent to the epithelial tissue and are thought to represent pre-cancerous lesions.
Endoscopic submucosal dissection (ESD) is an advanced surgical procedure using endoscopy to remove gastrointestinal tumors that have not entered the muscle layer. ESD may be done in the esophagus, stomach or colon. Application of endoscopic resection (ER) to gastrointestinal (GI) neoplasms is limited to lesions with no risk of nodal metastasis. Either polypectomy or endoscopic mucosal resection (EMR) is beneficial for patients because of its low level of invasiveness. However, to ensure the curative potential of these treatment modalities, accurate histopathologic assessment of the resected specimens is essential because the depth of invasion and lymphovascular infiltration of the tumor is associated with considerable risk for lymph node metastasis. For accurate assessment of the appropriateness of the therapy, en bloc resection is more desirable than piecemeal resection. For a reliable en bloc resection of GI neoplasms, a new method of ER called endoscopic submucosal dissection (ESD) has been developed.
Serrated polyposis syndrome (SPS), previously known as hyperplastic polyposis syndrome, is a disorder characterized by the appearance of serrated polyps in the colon. While serrated polyposis syndrome does not cause symptoms, the condition is associated with a higher risk of colorectal cancer (CRC). The lifelong risk of CRC is between 25 and 40%. SPS is the most common polyposis syndrome affecting the colon, but is under recognized due to a lack of systemic long term monitoring. Diagnosis requires colonoscopy, and is defined by the presence of either of two criteria: ≥5 serrated lesions/polyps proximal to the rectum, or >20 serrated lesions/polyps of any size distributed throughout the colon with 5 proximal to the rectum.
Postpolypectomy coagulation syndrome is a condition that occurs following colonoscopy with electrocautery polypectomy, which results in a burn injury to the wall of the gastrointestinal tract. The condition results in abdominal pain, fever, elevated white blood cell count and elevated serum C-reactive protein.

Kenneth Frank Binmoeller is a medical doctor and author of multiple scientific contributions and over 300 publications, as well as the inventor of the lumen-apposing metal stent (LAMS) and AXIOS System. These are medical devices used to relieve blockages while creating a direct connection between two bodily structures. He practices in the field of Gastroenterology with a specialty of Advanced Endoscopic Intervention. Binmoeller has been published for his innovations in medical devices and training in the field of Endoscopy.
References
- 1 2 Han KS, Sohn DK, Choi DH, et al. (January 2008). "Prolongation of the period between biopsy and EMR can influence the nonlifting sign in endoscopically resectable colorectal cancers". Gastrointest. Endosc. 67 (1): 97–102. doi:10.1016/j.gie.2007.05.057. PMID 18155430.
- ↑ Uno Y, Munakata A (1994). "The non-lifting sign of invasive colon cancer". Gastrointest. Endosc. 40 (4): 485–9. doi:10.1016/S0016-5107(94)70216-0. PMID 7926542.
- ↑ Ishiguro A, Uno Y, Ishiguro Y, Munakata A, Morita T (September 1999). "Correlation of lifting versus non-lifting and microscopic depth of invasion in early colorectal cancer". Gastrointest. Endosc. 50 (3): 329–33. doi:10.1053/ge.1999.v50.98591. PMID 10462651.
- ↑ Kobayashi N, Saito Y, Sano Y, et al. (August 2007). "Determining the treatment strategy for colorectal neoplastic lesions: endoscopic assessment or the non-lifting sign for diagnosing invasion depth?". Endoscopy . 39 (8): 701–5. doi:10.1055/s-2007-966587. PMID 17661244. S2CID 260133918.