Related Research Articles

A brain tumor occurs when abnormal cells form within the brain. There are two main types of tumors: malignant (cancerous) tumors and benign (non-cancerous) tumors. These can be further classified as primary tumors, which start within the brain, and secondary tumors, which most commonly have spread from tumors located outside the brain, known as brain metastasis tumors. All types of brain tumors may produce symptoms that vary depending on the size of the tumor and the part of the brain that is involved. Where symptoms exist, they may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking, with sensations, or unconsciousness.

Photodynamic therapy (PDT) is a form of phototherapy involving light and a photosensitizing chemical substance used in conjunction with molecular oxygen to elicit cell death (phototoxicity).

Tumor hypoxia is the situation where tumor cells have been deprived of oxygen. As a tumor grows, it rapidly outgrows its blood supply, leaving portions of the tumor with regions where the oxygen concentration is significantly lower than in healthy tissues. Hypoxic microenvironments in solid tumors are a result of available oxygen being consumed within 70 to 150 μm of tumor vasculature by rapidly proliferating tumor cells thus limiting the amount of oxygen available to diffuse further into the tumor tissue. In order to support continuous growth and proliferation in challenging hypoxic environments, cancer cells are found to alter their metabolism. Furthermore, hypoxia is known to change cell behavior and is associated with extracellular matrix remodeling and increased migratory and metastatic behavior.
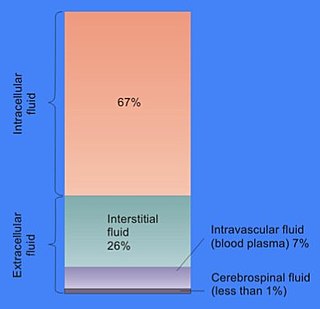
In cell biology, extracellular fluid (ECF) denotes all body fluid outside the cells of any multicellular organism. Total body water in healthy adults is about 50–60% of total body weight; women and the obese typically have a lower percentage than lean men. Extracellular fluid makes up about one-third of body fluid, the remaining two-thirds is intracellular fluid within cells. The main component of the extracellular fluid is the interstitial fluid that surrounds cells.

Glioblastoma, previously known as glioblastoma multiforme (GBM), is the most aggressive and most common type of cancer that originates in the brain, and has a very poor prognosis for survival. Initial signs and symptoms of glioblastoma are nonspecific. They may include headaches, personality changes, nausea, and symptoms similar to those of a stroke. Symptoms often worsen rapidly and may progress to unconsciousness.

Tirapazamine is an experimental anticancer drug that is activated to a toxic radical only at very low levels of oxygen (hypoxia). Such levels are common in human solid tumors, a phenomenon known as tumor hypoxia. Thus, tirapazamine is activated to its toxic form preferentially in the hypoxic areas of solid tumors. Cells in these regions are resistant to killing by radiotherapy and most anticancer drugs. Thus the combination of tirapazamine with conventional anticancer treatments is particularly effective. As of 2006, tirapazamine is undergoing phase III testing in patients with head and neck cancer and gynecological cancer, and similar trials are being undertaken for other solid tumor types.
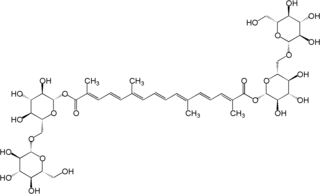
Crocin is a carotenoid chemical compound that is found in the flowers of crocus and gardenia. Its oxygen content also chemically makes it a xanthene. Crocin is the chemical primarily responsible for the color of saffron.

Crocetin is a natural apocarotenoid dicarboxylic acid that is found in the crocus flower together with its glycoside, crocin, and Gardenia jasminoides fruits. It is also known as crocetic acid. It forms brick red crystals with a melting point of 285 °C.
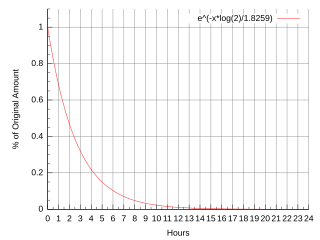
Fluorine-18 (18F) is a fluorine radioisotope which is an important source of positrons. It has a mass of 18.0009380(6) u and its half-life is 109.771(20) minutes. It decays by positron emission 96.7% of the time and electron capture 3.3% of the time. Both modes of decay yield stable oxygen-18.

Evofosfamide. Is a compound being evaluated in clinical trials for the treatment of multiple tumor types as a monotherapy and in combination with chemotherapeutic agents and other targeted cancer drugs.
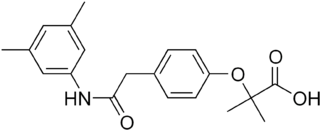
Efaproxiral (INN) is an analogue of the cholesterol drug bezafibrate developed for the treatment of depression, traumatic brain injury, ischemia, stroke, myocardial infarction, diabetes, hypoxia, sickle cell disease, hypercholesterolemia and as a radio sensitiser.
A radiosensitizer is an agent that makes tumor cells more sensitive to radiation therapy. It is sometimes also known as a radiation sensitizer or radio-enhancer.

Temozolomide, sold under the brand name Temodar among others, is an anticancer medication used to treat brain tumors such as glioblastoma and anaplastic astrocytoma. It is taken by mouth or via intravenous infusion.

Sonodynamic therapy (SDT) is a noninvasive treatment, often used for tumor irradiation, that utilizes a sonosensitizer and the deep penetration of ultrasound to treat lesions of varying depths by reducing target cell number and preventing future tumor growth. Many existing cancer treatment strategies cause systemic toxicity or cannot penetrate tissue deep enough to reach the entire tumor; however, emerging ultrasound stimulated therapies could offer an alternative to these treatments with their increased efficiency, greater penetration depth, and reduced side effects. Sonodynamic therapy could be used to treat cancers and other diseases, such as atherosclerosis, and diminish the risk associated with other treatment strategies since it induces cytotoxic effects only when externally stimulated by ultrasound and only at the cancerous region, as opposed to the systemic administration of chemotherapy drugs.

Diffusion Pharmaceuticals Inc (NASDAQ:DFFN) is a publicly traded biotechnology and drug development company based in Charlottesville, Virginia, U.S. It was co-founded in 2001 by American life sciences entrepreneur David Kalergis and University of Virginia Chemical Engineering Professor John L. Gainer. Gainer is the inventor of the company's platform technology of oxygen diffusion-enhancing compounds and its lead drug, trans sodium crocetinate (TSC). TSC acts to increase the rate at which oxygen moves through blood plasma by the process of diffusion, a phenomenon that forms the basis for the company's name. On January 8, 2016, the formerly privately held company merged with Restorgenex Corporation to become a publicly traded NASDAQ-listed company with the trading symbol DFFN. TSC and other oxygen diffusion-enhancing compounds, including bipolar trans carotenoid salts, have been investigated by Diffusion Pharmaceuticals for treatment of conditions associated with reduced oxygen availability in tissues (hypoxia). Most recently, Diffusion has begun the initiation of clinical trials in the U.S. and Eastern Europe for the use of trans sodium crocetinate in the treatment of COVID-19 patients with respiratory distress-related oxygen deficiency and the risk of multiple organ failure.

John L. Gainer is an American chemical engineer and co-founder and former chief scientific officer of Diffusion Pharmaceuticals, a biotechnology and pharmaceutical company based in Charlottesville, Virginia, U.S. Professor Gainer retired from his position as Chief Science Officer of Diffusion Pharmaceuticals in March, 2020. Gainer pioneered investigation into the mechanism of action underlying oxygen diffusion-enhancing compounds (ODECs) and invented the subclass of ODECs known as bipolar trans carotenoid salts. The lead compound of this class is trans sodium crocetinate (TSC) which Gainer invented while a professor of chemical engineering at the University of Virginia.

David Kalergis is an American life sciences entrepreneur and the co-founder and chair of Atelerix Life Sciences Inc., a Charlottesville, Virginia, U.S.-based biotechnology and pharmaceutical company developing novel treatments for the reversal of opioid induced respiratory depression. He co-founded the company in 2020 with Stephen Lewis, PhD, James Bates, MD/PhD, and Ben Gaston, MD.
Carotenoid complexes are physical associations of carotenoids with other molecules.

Furegrelate, also known as 5-(3-pyridinylmethyl)benzofurancarboxylic acid, is a chemical compound with thromboxane enzyme inhibiting properties that was originally developed by Pharmacia Corporation as a drug to treat arrhythmias, ischaemic heart disorders, and thrombosis but was discontinued. It is commercially available in the form furegrelate sodium salt.
Boron neutron capture therapeutics are pharmaceuticals used to deliver boron-10 to cancerous cells as part of boron neutron capture therapy (BNCT). Boron-10 atoms strongly absorb neutrons to form a metastable state of boron-11, which undergoes α-decay. By accumulating boron-10 in cancerous cells and subjecting the tumor to neutron radiation, high-energy α particles are selectively delivered only to the target cells. In order for BNCT to be effective, safe, and successful, therapeutic candidates must be non-toxic, must selectively accumulate in target tissue and not normal tissue, and must remain in target tissue while fading from the blood stream. As of 2023, the technology is available in Japan only, and even there few implementations have been reported.
References
- 1 2 3 USpatent 8206751,Gainer J,"New Class of Therapeutics that Enhance Small Molecule Diffusion",issued 2009-04-30
- 1 2 3 4 Gainer, J (2008). "Trans-sodium crocetinate for treating hypoxia/ischemia". Expert Opinion on Investigational Drugs. 17 (6): 917–924. doi:10.1517/13543784.17.6.917. PMID 18491992. S2CID 71663644.
- ↑ Gainer J; G.M. Chisolm III (1974). "Oxygen diffusion and atherosclerosis". Atherosclerosis. 19 (1): 135–138. doi:10.1016/0021-9150(74)90049-5. PMID 4810465.
- ↑ Abdullaev F, Espinosa-Aguirre J (2004). "Biomedical properties of saffron and its potential use in cancer therapy and chemoprevention trials". Cancer Detection and Prevention. 28 (6): 426–432. doi:10.1016/j.cdp.2004.09.002. PMID 15582266.
- ↑ Lapchak P (2010). "Efficacy and safety profile of the carotenoid trans sodium crocetinate administered to rabbits following multiple infarct ischemic strokes: A combination therapy study with tissue plasminogen activator". Brain Research. 1309: 136–145. doi:10.1016/j.brainres.2009.10.067. PMID 19891959. S2CID 25369069.
- 1 2 "Safety and Efficacy Study of Trans Sodium Crocetinate (TSC) With Concomitant Radiation Therapy and Temozolomide in Newly Diagnosed Glioblastoma (GBM)". ClinicalTrials.gov. November 2011. Retrieved 18 September 2012.
- ↑ Sheehan, Jason; et al. (2008). "Use of trans sodium crocetinate for sensitizing glioblastoma multiforme to radiation". Journal of Neurosurgery. 108 (5): 972–978. doi:10.3171/JNS/2008/108/5/0972. PMID 18447715.
- ↑ "Diffusion Pharmaceuticals Announces FDA Accelerated Review of TSC Clinical Development Plan to Treat COVID-19 Patients with ARDS". Diffusion Pharmaceuticals. May 5, 2020. Retrieved May 25, 2020.
- 1 2 3 USpatent 7919527,Gainer J&Grabiak R,"Bipolar trans carotenoid salts and their uses",issued 2011-04-05
- 1 2 Laidig, K.E., J.L. Gainer, V. Daggett (1998). "Altering Diffusivity in Biological Solutions through Modification of Solution Structure and Dynamics". Journal of the American Chemical Society. 120 (36): 9394–9395. doi:10.1021/ja981656j.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - 1 2 Cannon, Joseph G (1999). Pharmacology for Chemists. New York: Oxford University Press. ISBN 978-0841235243.
- ↑ Manabe H, et al. (2010). "Protection against focal ischemic injury to the brain by trans-sodium crocetinate". Journal of Neurosurgery. 113 (4): 802–809. doi:10.3171/2009.10.JNS09562. PMC 3380430 . PMID 19961314.
- ↑ Starr, Cecie; McMillan, Beverly (2012). Human Biology (9th ed.). Cengage Learning. ISBN 978-0840061669.