Related Research Articles
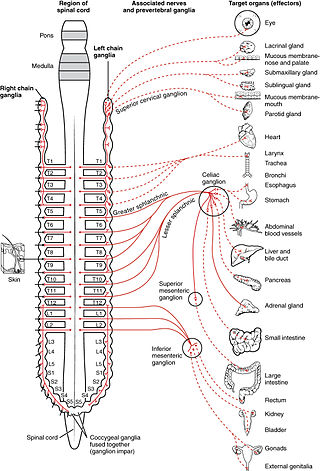
The sympathetic nervous system (SNS) is one of the three divisions of the autonomic nervous system, the others being the parasympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.
Functional abdominal pain syndrome (FAPS), chronic functional abdominal pain (CFAP), or centrally mediated abdominal pain syndrome (CMAP) is a pain syndrome of the abdomen, that has been present for at least six months, is not well connected to gastrointestinal function, and is accompanied by some loss of everyday activities. The discomfort is persistent, near-constant, or regularly reoccurring. The absence of symptom association with food intake or defecation distinguishes functional abdominal pain syndrome from other functional gastrointestinal illnesses, such as irritable bowel syndrome (IBS) and functional dyspepsia.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true anaesthesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.

A thoracotomy is a surgical procedure to gain access into the pleural space of the chest. It is performed by surgeons to gain access to the thoracic organs, most commonly the heart, the lungs, or the esophagus, or for access to the thoracic aorta or the anterior spine. A thoracotomy is the first step in thoracic surgeries including lobectomy or pneumonectomy for lung cancer or to gain thoracic access in major trauma.
Endoscopic thoracic sympathectomy (ETS) is a surgical procedure in which a portion of the sympathetic nerve trunk in the thoracic region is destroyed. ETS is used to treat excessive sweating in certain parts of the body, facial blushing, Raynaud's disease and reflex sympathetic dystrophy. By far the most common complaint treated with ETS is sweaty palms. The intervention is controversial and illegal in some jurisdictions. Like any surgical procedure, it has risks; the endoscopic sympathetic block (ESB) procedure and those procedures that affect fewer nerves have lower risks.

The stellate ganglion is a sympathetic ganglion formed by the fusion of the inferior cervical ganglion and the first thoracic ganglion, which is present in 80% of individuals. Sometimes, the second and the third thoracic ganglia are included in this fusion.

Nerve block or regional nerve blockade is any deliberate interruption of signals traveling along a nerve, often for the purpose of pain relief. Local anesthetic nerve block is a short-term block, usually lasting hours or days, involving the injection of an anesthetic, a corticosteroid, and other agents onto or near a nerve. Neurolytic block, the deliberate temporary degeneration of nerve fibers through the application of chemicals, heat, or freezing, produces a block that may persist for weeks, months, or indefinitely. Neurectomy, the cutting through or removal of a nerve or a section of a nerve, usually produces a permanent block. Because neurectomy of a sensory nerve is often followed, months later, by the emergence of new, more intense pain, sensory nerve neurectomy is rarely performed.

Spinal fusion, also called spondylodesis or spondylosyndesis, is a surgery performed by orthopaedic surgeons or neurosurgeons that joins two or more vertebrae. This procedure can be performed at any level in the spine and prevents any movement between the fused vertebrae. There are many types of spinal fusion and each technique involves using bone grafting—either from the patient (autograft), donor (allograft), or artificial bone substitutes—to help the bones heal together. Additional hardware is often used to hold the bones in place while the graft fuses the two vertebrae together. The placement of hardware can be guided by fluoroscopy, navigation systems, or robotics.

A rib fracture is a break in a rib bone. This typically results in chest pain that is worse with inspiration. Bruising may occur at the site of the break. When several ribs are broken in several places a flail chest results. Potential complications include a pneumothorax, pulmonary contusion, and pneumonia.

The triangle of auscultation is a relative thinning of the musculature of the back, situated along the medial border of the scapula which allows for improved listening to the lungs.
Abdominal angina is abdominal pain after eating that occurs in individuals with ongoing poor blood supply to their small intestines known as chronic mesenteric ischemia. Although the term angina alone usually denotes angina pectoris, angina by itself can also mean "any spasmodic, choking, or suffocative pain", with an anatomic adjective defining its focus; so, in this case, spasmodic pain in the abdomen. Stedman's Medical Dictionary Online defines abdominal angina as "intermittent abdominal pain, frequently occurring at a fixed time after eating, caused by inadequacy of the mesenteric circulation resulting from arteriosclerosis or other arterial disease. Synonym: intestinal angina."
The Outcomes Research Consortium is an international clinical research group that focuses on the perioperative period, along with critical care and pain management. The Consortium's aim is to improve the quality of care for surgical, critical care, and chronic pain patients and to "Provide the evidence for evidence-based practice." Members of the Consortium are especially interested in testing simple, low-risk, and inexpensive treatments that have the potential to markedly improve patients' surgical experiences.
Continuous wound infiltration (CWI) refers to the continuous infiltration of a local anesthetic into a surgical wound to aid in pain management during post-operative recovery.

A double-lumen endotracheal tube is a type of endotracheal tube which is used in tracheal intubation during thoracic surgery and other medical conditions to achieve selective, one-sided ventilation of either the right or the left lung.

Intercostal nerve block is a nerve block which temporarily or permanently interrupts the flow of signals along an intercostal nerve, usually performed to relieve pain.

Vijaipal Singh in Narsan Kalan, Haridwar District of Uttarakhand State, India is an Agricultural scientist associated with the Indian Council of Agricultural Research (ICAR) and is known for his contributions to the science of rice genetics and breeding. He is well known for his contributions in developing the most popular Basmati rice variety, Pusa Basmati 1121. A post graduate and a doctoral degree (PhD) holder in Agriculture Botany from Agra University, he started his career as a research assistant at the Indian Agricultural Research Institute (IARI), New Delhi in 1968 and retired as a professor at the Division of Genetics, IARI. Singh is credited with several articles published in peer reviewed journals. In recognition of his services to the nation, he was honored by the Government of India, in 2012, with the fourth highest Indian civilian award of Padma Shri.
Pectoralis minor syndrome (PMS) is a condition related to thoracic outlet syndrome (TOS) that results from the pectoralis minor muscle being too tight. PMS results from the brachial plexus being compressed under the pectoralis minor while TOS involves compression of the bundle above the clavicle. In most patients, the nerves are constricted resulting in neurogenic PMS, but venous compression can also occur.

Renal infarction is a medical condition caused by an abrupt disruption of the renal blood flow in either one of the segmental branches or the major ipsilateral renal artery. Patients who have experienced an acute renal infarction usually report sudden onset flank pain, which is often accompanied by fever, nausea, and vomiting.
Post-mastectomy pain syndrome (PMPS) is used to describe persistent neuropathic pain that follows breast surgery, such as mastectomy and lumpectomy. PMPS manifests as consent pain and unusual sensations in the upper and lateral thoracic, axilla, and medial and posterior arm and shoulder intercostal nerve distribution region.
References
- ↑ Batra, Krishnan & Agarwal.
- ↑ Ardon et al. 2020, pp. 394–400.
- ↑ D’Ercole, Arora & Kumar 2018, pp. 915–927.
- ↑ Slinchenkova et al. 2023, pp. 203–208.
- ↑ Tighe, Greene & Rajadurai 2010, pp. 133–137.
- ↑ Karmakar 2001, pp. 771–780.