Related Research Articles

Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV) is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

Positive airway pressure (PAP) is a mode of respiratory ventilation used in the treatment of sleep apnea. PAP ventilation is also commonly used for those who are critically ill in hospital with respiratory failure, in newborn infants (neonates), and for the prevention and treatment of atelectasis in patients with difficulty taking deep breaths. In these patients, PAP ventilation can prevent the need for tracheal intubation, or allow earlier extubation. Sometimes patients with neuromuscular diseases use this variety of ventilation as well. CPAP is an acronym for "continuous positive airway pressure", which was developed by Dr. George Gregory and colleagues in the neonatal intensive care unit at the University of California, San Francisco. A variation of the PAP system was developed by Professor Colin Sullivan at Royal Prince Alfred Hospital in Sydney, Australia, in 1981.

Spirometry is the most common of the pulmonary function tests (PFTs). It measures lung function, specifically the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is helpful in assessing breathing patterns that identify conditions such as asthma, pulmonary fibrosis, cystic fibrosis, and COPD. It is also helpful as part of a system of health surveillance, in which breathing patterns are measured over time.

Respiratory arrest is a serious medical condition caused by apnea or respiratory dysfunction severe enough that it will not sustain the body. Prolonged apnea refers to a patient who has stopped breathing for a long period of time. If the heart muscle contraction is intact, the condition is known as respiratory arrest. An abrupt stop of pulmonary gas exchange lasting for more than five minutes may permanently damage vital organs, especially the brain. Lack of oxygen to the brain causes loss of consciousness. Brain injury is likely if respiratory arrest goes untreated for more than three minutes, and death is almost certain if more than five minutes.
Dual-control modes of ventilation are auto-regulated pressure-controlled modes of mechanical ventilation with a user-selected tidal volume target. The ventilator adjusts the pressure limit of the next breath as necessary according to the previous breath's measured exhaled tidal volume. Peak airway pressure varies from breath to breath according to changes in the patient's airway resistance and lung compliance.
Positive end-expiratory pressure (PEEP) is the pressure in the lungs above atmospheric pressure that exists at the end of expiration. The two types of PEEP are extrinsic PEEP and intrinsic PEEP. Pressure that is applied or increased during an inspiration is termed pressure support.PEEP is a therapeutic parameter set in the ventilator, or a complication of mechanical ventilation with air trapping (auto-PEEP).
High-frequency ventilation is a type of mechanical ventilation which utilizes a respiratory rate greater than four times the normal value. and very small tidal volumes. High frequency ventilation is thought to reduce ventilator-associated lung injury (VALI), especially in the context of ARDS and acute lung injury. This is commonly referred to as lung protective ventilation. There are different types of high-frequency ventilation. Each type has its own unique advantages and disadvantages. The types of HFV are characterized by the delivery system and the type of exhalation phase.
Lung compliance, or pulmonary compliance, is a measure of the lung's ability to stretch and expand. In clinical practice it is separated into two different measurements, static compliance and dynamic compliance. Static lung compliance is the change in volume for any given applied pressure. Dynamic lung compliance is the compliance of the lung at any given time during actual movement of air.
Cricoid pressure, also known as the Sellick manoeuvre or Sellick maneuver, is a technique used in endotracheal intubation to try to reduce the risk of regurgitation. The technique involves the application of pressure to the cricoid cartilage at the neck, thus occluding the esophagus which passes directly behind it.

Airway pressure release ventilation (APRV) is a pressure control mode of mechanical ventilation that utilizes an inverse ratio ventilation strategy. APRV is an applied continuous positive airway pressure (CPAP) that at a set timed interval releases the applied pressure. Depending on the ventilator manufacturer, it may be referred to as BiVent. This is just as appropriate to use, since the only difference is that the term APRV is copyrighted.

A liquid ventilator is similar to a medical ventilator except that it should be able to ensure reliable total liquid ventilation with a breatheable liquid ·. Liquid ventilators are prototypes that may have been used for animal experimentations but experts recommend continued development of a liquid ventilator toward clinical applications.

Heated humidified high-flow therapy, often simply called high flow therapy, is a type of respiratory support that delivers a flow of medical gas to a patient of up to 60 liters per minute and 100% oxygen through a large bore or high flow nasal cannula. Primarily studied in neonates, it has also been found effective in some adults to treat hypoxemia and work of breathing issues. The key components of it are a gas blender, heated humidifier, heated circuit, and cannula.
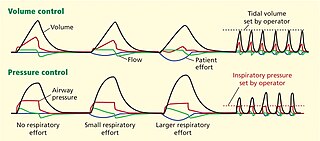
Modes of mechanical ventilation are one of the most important aspects of the usage of mechanical ventilation. The mode refers to the method of inspiratory support. In general, mode selection is based on clinician familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There have been substantial changes in the nomenclature of mechanical ventilation over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy.
ΔP is a mathematical term symbolizing a change (Δ) in pressure (P).
Many terms are used in mechanical ventilation, some are specific to brand, model, trademark and mode of mechanical ventilation. There is a standardized nomenclature of mechanical ventilation that is specific about nomenclature related to modes, but not settings and variables.
Intermittent Mandatory Ventilation (IMV) refers to any mode of mechanical ventilation where a regular series of breaths are scheduled but the ventilator senses patient effort and reschedules mandatory breaths based on the calculated need of the patient. Similar to continuous mandatory ventilation in parameters set for the patients pressures and volumes but distinct in its ability to support a patient by either supporting their own effort or providing support when patient effort is not sensed. IMV is frequently paired with additional strategies to improve weaning from ventilator support or to improve cardiovascular stability in patients who may need full life support.
Inverse ratio ventilation (IRV) is not necessarily a mode of mechanical ventilation though it may be referred to as such. IRV is a strategy of ventilating the lungs in such a way that the amount of time the lungs are in inhalation is greater than the amount of time they are in exhalation, allowing for a constant inflation of the lungs, ensuring they remain "recruited". The primary goal for IRV is improved oxygenation by forcing inspiratory time to be greater than expiratory time increasing the mean airway pressure and potentially improving oxygenation. Normal I:E ratio is 5:6, so forcing the I:E to be 2:1, 3:1, 4:1, is the source of the term for the strategy.
Mean airway pressure typically refers to the mean pressure applied during positive-pressure mechanical ventilation. Mean airway pressure correlates with alveolar ventilation, arterial oxygenation, hemodynamic performance, and barotrauma. It can also match the alveolar pressure if there is no difference between inspiratory and expiratory resistance.
A respiratory pressure meter measures the maximum inspiratory and expiratory pressures that a patient can generate at either the mouth (MIP and MEP) or inspiratory pressure a patient can generate through their nose via a sniff manoeuvre (SNIP). These measurements require patient cooperation and are known as volitional tests of respiratory muscle strength. Handheld devices displaying the measurement achieved in cmH2O and the pressure trace created, allow quick patient testing away from the traditional pulmonary laboratory and are useful for ward based, out patient, and preoperative assessment as well as for use by pulmonologists and physiotherapists.

Pendelluft refers to the movement of gas between two regions of the lung, usually between regions of differing compliance or airway resistance. Pendelluft is an important physiological concept to take into account during mechanical ventilation, particularly in patients with an open thorax, severe bronchospasm, or with heterogeneous lung compliance. It was first published as a physiological concept in 1956.
References
- ↑ Rose, Louise (2010). "Clinical application of ventilator modes: Ventilatory strategies for lung protection". Australian Critical Care. 23 (2): 71–80. doi:10.1016/j.aucc.2010.03.003. PMID 20378369.
- ↑ Sarkar, Subrata; Donn, Steven M. (2007). "In Support of Pressure Support". Clinics in Perinatology. 34 (1): 117–128. doi:10.1016/j.clp.2006.12.010. PMID 17394934.