The prostate is both an accessory gland of the male reproductive system and a muscle-driven mechanical switch between urination and ejaculation. It is found only in some mammals. It differs between species anatomically, chemically, and physiologically. Anatomically, the prostate is found below the bladder, with the urethra passing through it. It is described in gross anatomy as consisting of lobes and in microanatomy by zone. It is surrounded by an elastic, fibromuscular capsule and contains glandular tissue as well as connective tissue.

Prostate cancer is cancer of the prostate. The prostate is a gland in the male reproductive system that surrounds the urethra just below the bladder. Most prostate cancers are slow growing. Cancerous cells may spread to other areas of the body, particularly the bones and lymph nodes. It may initially cause no symptoms. In later stages, symptoms include pain or difficulty urinating, blood in the urine, or pain in the pelvis or back. Benign prostatic hyperplasia may produce similar symptoms. Other late symptoms include fatigue, due to low levels of red blood cells.

Carcinoma is a malignancy that develops from epithelial cells. Specifically, a carcinoma is a cancer that begins in a tissue that lines the inner or outer surfaces of the body, and that arises from cells originating in the endodermal, mesodermal or ectodermal germ layer during embryogenesis.
In medicine, Breslow's depth was used as a prognostic factor in melanoma of the skin. It is a description of how deeply tumor cells have invaded. Currently, the standard Breslow's depth has been replaced by the AJCC depth, in the AJCC staging system of melanoma. Originally, Breslow's depth was divided into 5 stages.
A mastocytoma or mast cell tumor is a type of round-cell tumor consisting of mast cells. It is found in humans and many animal species; it also can refer to an accumulation or nodule of mast cells that resembles a tumor.

A malignant peripheral nerve sheath tumor (MPNST) is a form of cancer of the connective tissue surrounding nerves. Given its origin and behavior it is classified as a sarcoma. About half the cases are diagnosed in people with neurofibromatosis; the lifetime risk for an MPNST in patients with neurofibromatosis type 1 is 8–13%. MPNST with rhabdomyoblastomatous component are called malignant triton tumors.

Pleomorphic adenoma is a common benign salivary gland neoplasm characterised by neoplastic proliferation of epithelial (ductal) cells along with myoepithelial components, having a malignant potentiality. It is the most common type of salivary gland tumor and the most common tumor of the parotid gland. It derives its name from the architectural Pleomorphism seen by light microscopy. It is also known as "Mixed tumor, salivary gland type", which refers to its dual origin from epithelial and myoepithelial elements as opposed to its pleomorphic appearance.
Prostate cancer staging is the process by which physicians categorize the risk of cancer having spread beyond the prostate, or equivalently, the probability of being cured with local therapies such as surgery or radiation. Once patients are placed in prognostic categories, this information can contribute to the selection of an optimal approach to treatment. Prostate cancer stage can be assessed by either clinical or pathological staging methods. Clinical staging usually occurs before the first treatment and tumour presence is determined through imaging and rectal examination, while pathological staging is done after treatment once a biopsy is performed or the prostate is removed by looking at the cell types within the sample.

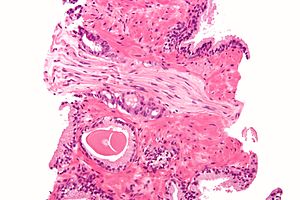
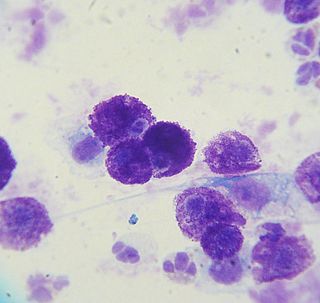
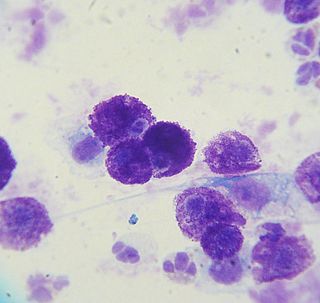
The Gleason grading system is used to help evaluate the prognosis of men with prostate cancer using samples from a prostate biopsy. Together with other parameters, it is incorporated into a strategy of prostate cancer staging which predicts prognosis and helps guide therapy. A Gleason score is given to prostate cancer based upon its microscopic appearance. Cancers with a higher Gleason score are more aggressive and have a worse prognosis. Pathological scores range from 2 to 10, with higher numbers indicating greater risks and higher mortality. The system is widely accepted and used for clinical decision making even as it is recognised that certain biomarkers, like ACP1 expression, might yield higher predictive value for future disease course.

Signet ring cell carcinoma (SRCC) is a rare form of highly malignant adenocarcinoma that produces mucin. It is an epithelial malignancy characterized by the histologic appearance of signet ring cells.

Leptomeningeal cancer is a rare complication of cancer in which the disease spreads from the original tumor site to the meninges surrounding the brain and spinal cord. This leads to an inflammatory response, hence the alternative names neoplastic meningitis (NM), malignant meningitis, or carcinomatous meningitis. The term leptomeningeal describes the thin meninges, the arachnoid and the pia mater, between which the cerebrospinal fluid is located. The disorder was originally reported by Eberth in 1870.
Douglas S. Scherr, M.D. is an American surgeon and specialist in Urologic Oncology. He is currently the Clinical Director of Urologic Oncology at the Weill Medical College of Cornell University in New York City. He also holds an appointment at the Rockefeller University in New York as a Visiting Associate Physician. Dr. Scherr was the first physician at Cornell to perform a robotic prostatectomy as well as a robotic cystectomy.

High-grade prostatic intraepithelial neoplasia (HGPIN) is an abnormality of prostatic glands and believed to precede the development of prostate adenocarcinoma.

In medicine, desmoplasia is the growth of fibrous or connective tissue. It is also called desmoplastic reaction to emphasize that it is secondary to an insult. Desmoplasia may occur around a neoplasm, causing dense fibrosis around the tumor, or scar tissue (adhesions) within the abdomen after abdominal surgery.
Mark S. Soloway is a leading authority in urologic cancer, researcher, former departmental Chair, medical professor and invitational lecturer. He served as Chairman of the University of Miami Miller School of Medicine Department of Urology and is currently a Professor at the Miller School of Medicine. Born in Cleveland, Soloway received his B.Sc. from Northwestern University in Chicago (1961–1964). He completed his M.D. and residency at Case Western Reserve University School of Medicine in Cleveland, Ohio (1964–1970). He completed a fellowship at the National Cancer Institute of the National Institute of Health in Bethesda, MD (1970–1972). Soloway has received numerous awards for his work as a researcher and teacher, These awards are American Urological Association's Gold Cystoscope award, Mosby Scholarship for Scholastic Excellence award (1967), North Central Section of American Urological Association Traveling Fellowship award (1972) and many others. These are outstanding achievements for an individual who has contributed most to the field of urology within ten years of completion of his residency program” (1984).

Lymphovascular invasion is the invasion of a cancer to the blood vessels and/or lymphatics.

Invasive urothelial carcinoma is a type of transitional cell carcinoma. It is a type of cancer that develops in the urinary system: the kidney, urinary bladder, and accessory organs. Transitional cell carcinoma is the most common type of bladder cancer and cancer of the ureter, urethra, renal pelvis, the ureters, the bladder, and parts of the urethra and urachus. It originates from tissue lining the inner surface of these hollow organs - transitional epithelium. The invading tumors can extend from the kidney collecting system to the bladder.
Carcinoma of the tonsil is a type of squamous cell carcinoma. The tonsil is the most common site of squamous cell carcinoma in the oropharynx. It comprises 23.1% of all malignancies of the oropharynx. The tumors frequently present at advanced stages, and around 70% of patients present with metastasis to the cervical lymph nodes. . The most reported complaints include sore throat, otalgia or dysphagia. Some patients may complain of feeling the presence of a lump in the throat. Approximately 20% patients present with a node in the neck as the only symptom.
Prognostic markers are biomarkers used to measure the progress of a disease in the patient sample. Prognostic markers are useful to stratify the patients into groups, guiding towards precise medicine discovery. The widely used prognostic markers in cancers include stage, size, grade, node and metastasis. In addition to these common markers, there are prognostic markers specific to different cancer types. For example estrogen level, progesterone and HER2 are markers specific to breast cancer patients. There is evidence showing that genes behaving as tumor suppressors or carcinogens could act as prognostic markers due to altered gene expression or mutation. Besides genetic biomarkers, there are also biomarkers that are detected in plasma or body fluid which can be metabolic or protein biomarkers.
A histopathologic diagnosis of prostate cancer is the discernment of whether there is a cancer in the prostate, as well as specifying any subdiagnosis of prostate cancer if possible. The histopathologic subdiagnosis of prostate cancer has implications for the possibility and methodology of any subsequent Gleason scoring. The most common histopathological subdiagnosis of prostate cancer is acinar adenocarcinoma, constituting 93% of prostate cancers. The most common form of acinar adenocarcinoma, in turn, is "adenocarcinoma, not otherwise specified", also termed conventional, or usual acinar adenocarcinoma.